Resources: Understanding Your Child's Diagnosis

At Horizon Neuropsychological Services, we understand that it can be an emotional experience for parents and caregivers to receive a diagnosis for their child. For some, it is liberating to finally be able to put words to what they have been observing, while for others, it may bring about feelings of sadness or uncertainty. Regardless of your place in this process, understanding your child’s diagnosis is the first step in moving forward and helping him or her become the best version of themselves in life.
It is our hope that you can use our website as a starting place in researching your child’s diagnosis. By clicking the drop-down button next to each diagnosis, you will find a brief summary of the diagnostic criteria, links to resources, and a list of recommended readings. If you do not see your child’s diagnosis below, please contact our office so we can provide you with the appropriate resources and reading materials.
Neurodevelopmental Disorders
Neurodevelopmental Disorders become symptomatic early in development (typically before entering into school), which can negatively impact a child’s social, emotional, behavioral, and academic functioning as they mature, as well as their ability to engage in the workforce and maintain interpersonal relationships later in life.
Intellectual Disabilities
Intellectual Disabilities are a set of diagnoses characterized by limitations across both cognitive functioning (i.e., reasoning, learning, problem solving) and adaptive functioning (i.e., social and practical skills that help one engage with the environment independently). For each diagnosis, symptoms can vary in terms of severity.
A diagnosis of Intellectual Disability is given to an individual age 5 or above who experiences limitations across both their cognitive functioning (i.e., reasoning, learning, problem solving) and adaptive functioning (i.e., social and practical skills that help one engage with the environment independently). According to the DSM-V, the classification of intellectual disability severity is as follows:
| Conceptual Domain | Social Domain | Practical Domain | |
|---|---|---|---|
| Mild | In preschool, there may be no obvious conceptual differences. For school-aged children and adults, there are difficulties in learning the academic skills needed to meet age-related expectations. In adults, there are also difficulties with abstract thinking, executive functioning, and short-term memory. | Compared with typically developing peers, the individual is immature in social interactions. For example, there may be difficulty in accurately perceiving peers’ social cues. There may be difficulties regulating emotions and behavior in an age-appropriate fashion. | Individuals need some support with complex daily living tasks in comparison to peers. In adulthood, supports typically involve grocery shopping, transportation, home and child-care organization, food preparation, and money management. Support is needed to raise a family. |
| Moderate | Throughout development, the individual's conceptual skills lag markedly behind those of peers. Ongoing assistance daily is needed to complete conceptual tasks of day-to-day life, and others may take over these responsibilities throughout the lifespan. | Friendships with typically developing peers are often affected by communication or social limitations. Significant social and communicative support is needed in work settings for success. | The individual can care for personal needs involving eating, dressing, toileting, and hygiene as an adult. However, with an extended period of instruction, the individual may become independent in these areas (with the continuation of reminders). |
| Severe | Attainment of concepts is limited (e.g., money, time, quantity). Caretakers provide extensive supports for problem-solving throughout life. | Spoken language is quite limited in terms of vocabulary and grammar. Speech may be single words or phrases, and communication is focused on the here-and-now within everyday events. Relationships may be limited to family members and acquaintances. | The individual requires support for daily living (e.g., meals, dressing, bathing, and toileting). The individual requires supervision at all times and cannot make responsible decisions regarding the wellbeing of self or others. |
| Profound | Conceptual skills generally involve the physical world rather than symbolic processes. The individual may use objects in goal-directed fashion for self-care, work, and recreation. Motor and sensory impairments may prevent functional use of objects even if certain visuospatial skills are intact (e.g., can match objects based on physical characteristics seen visually, but cannot translate to appropriate use). | The individual has a minimal understanding of speech or gesture. He or she may understand some simple instructions or gestures, and express his or her desire and emotions largely through nonverbal, non-symbolic communication. The individual enjoys relationships with well-known family members and caretakers primarily. | The individual is dependent on others for all aspects of daily living. Although, individuals without severe physical impairments may assist with some daily work tasks at home, like carrying dishes to the table. Simple actions with objects may be the basis of participation in some vocational activities with high levels of ongoing support. |
Please visit the following sites for more information regarding Intellectual Disability (Intellectual Developmental Disorder):
http://www.aaidd.org/intellectual-disability/definition
https://www.psychiatry.org/patients-families/intellectual-disability/what-is-intellectual-disability
https://www.cdc.gov/ncbddd/developmentaldisabilities/facts-about-intellectual-disability.html
https://www.specialolympics.org/about/intellectual-disabilities/what-is-intellectual-disability
Book Recommendations:
Intellectual Disability : A Guide for Families and Professionals by James C. Harris
A Parent's Guide to Developmental Delays: Recognizing and Coping with Missed Milestones in Speech, Movement, Learning, and Other Areas by Laurie Fivozinsky LeComer
The Life We Never Expected: Hopeful Reflections on the Challenges of Parenting Children with Special Needs by Andrew Wilson
Global Developmental Delay is diagnosed when a child under the age of 5 is not appropriately meeting developmental milestones across several domains. When this diagnosis is given, it is imperative that the child is tested again at a later date to determine whether their weaknesses are simply a delay and have since improved with intervention, or whether their weaknesses have persisted and are more appropriately classified as a disability.
Internet Resources:
Resources vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Professionals diagnose Unspecified Intellectual Disability when an individual age 5 or above is not appropriately meeting developmental milestones across several domains and test findings are inconclusive. Reasons for inconclusive results can vary, but are usually due to the child’s inability or unwillingness to engage in testing procedures. When this occurs, it is important for parents and the evaluator to collaborate on ways to remove these barriers to testing and then reevaluate at a later date.
Internet Resources:
Resources vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Intellectual Disabilities
Intellectual Disabilities are a set of diagnoses characterized by limitations across both cognitive functioning (i.e., reasoning, learning, problem solving) and adaptive functioning (i.e., social and practical skills that help one engage with the environment independently). For each diagnosis, symptoms can vary in terms of severity.
A diagnosis of Intellectual Disability is given to an individual age 5 or above who experiences limitations across both their cognitive functioning (i.e., reasoning, learning, problem solving) and adaptive functioning (i.e., social and practical skills that help one engage with the environment independently). According to the DSM-V, the classification of intellectual disability severity is as follows:
| Mild (Conceptual Domain) In preschool, there may be no obvious conceptual differences. For school-aged children and adults, there are difficulties in learning the academic skills needed to meet age-related expectations. In adults, there are also difficulties with abstract thinking, executive functioning, and short-term memory. | Mild (Social Domain) Compared with typically developing peers, the individual is immature in social interactions. For example, there may be difficulty in accurately perceiving peers’ social cues. There may be difficulties regulating emotions and behavior in an age-appropriate fashion. | Mild (Practical Domain) Individuals need some support with complex daily living tasks in comparison to peers. In adulthood, supports typically involve grocery shopping, transportation, home and child-care organization, food preparation, and money management. Support is needed to raise a family. |
| Moderate (Conceptual Domain) Throughout development, the individual's conceptual skills lag markedly behind those of peers. Ongoing assistance daily is needed to complete conceptual tasks of day-to-day life, and others may take over these responsibilities throughout the lifespan. | Moderate (Social Domain) Friendships with typically developing peers are often affected by communication or social limitations. Significant social and communicative support is needed in work settings for success. | Moderate (Practical Domain) The individual can care for personal needs involving eating, dressing, toileting, and hygiene as an adult. However, with an extended period of instruction, the individual may become independent in these areas (with the continuation of reminders). |
| Severe (Conceptual Domain) Attainment of concepts is limited (e.g., money, time, quantity). Caretakers provide extensive supports for problem-solving throughout life. | Severe (Social Domain) Spoken language is quite limited in terms of vocabulary and grammar. Speech may be single words or phrases, and communication is focused on the here-and-now within everyday events. Relationships may be limited to family members and acquaintances. | Severe (Practical Domain) The individual requires support for daily living (e.g., meals, dressing, bathing, and toileting). The individual requires supervision at all times and cannot make responsible decisions regarding the wellbeing of self or others. |
| Profound (Conceptual Domain) Conceptual skills generally involve the physical world rather than symbolic processes. The individual may use objects in goal-directed fashion for self-care, work, and recreation. Motor and sensory impairments may prevent functional use of objects even if certain visuospatial skills are intact (e.g., can match objects based on physical characteristics seen visually, but cannot translate to appropriate use). | Profound (Social Domain) The individual has a minimal understanding of speech or gesture. He or she may understand some simple instructions or gestures, and express his or her desire and emotions largely through nonverbal, non-symbolic communication. The individual enjoys relationships with well-known family members and caretakers primarily. | Profound (Practical Domain) The individual is dependent on others for all aspects of daily living. Although, individuals without severe physical impairments may assist with some daily work tasks at home, like carrying dishes to the table. Simple actions with objects may be the basis of participation in some vocational activities with high levels of ongoing support. |
Please visit the following sites for more information regarding Intellectual Disability (Intellectual Developmental Disorder):
http://www.aaidd.org/intellectual-disability/definition
https://www.psychiatry.org/patients-families/intellectual-disability/what-is-intellectual-disability
https://www.cdc.gov/ncbddd/developmentaldisabilities/facts-about-intellectual-disability.html
https://www.specialolympics.org/about/intellectual-disabilities/what-is-intellectual-disability
Book Recommendations:
Intellectual Disability : A Guide for Families and Professionals by James C. Harris
A Parent's Guide to Developmental Delays: Recognizing and Coping with Missed Milestones in Speech, Movement, Learning, and Other Areas by Laurie Fivozinsky LeComer
The Life We Never Expected: Hopeful Reflections on the Challenges of Parenting Children with Special Needs by Andrew Wilson
Global Developmental Delay is diagnosed when a child under the age of 5 is not appropriately meeting developmental milestones across several domains. When this diagnosis is given, it is imperative that the child is tested again at a later date to determine whether their weaknesses are simply a delay and have since improved with intervention, or whether their weaknesses have persisted and are more appropriately classified as a disability.
Internet Resources:
Resources vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Professionals diagnose Unspecified Intellectual Disability when an individual age 5 or above is not appropriately meeting developmental milestones across several domains and test findings are inconclusive. Reasons for inconclusive results can vary, but are usually due to the child’s inability or unwillingness to engage in testing procedures. When this occurs, it is important for parents and the evaluator to collaborate on ways to remove these barriers to testing and then reevaluate at a later date.
Internet Resources:
Resources vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Communication Disorders
Communication Disorders are a set of diagnoses involving impairment in the ability to understand and/or communicate with others. Difficulties may include both verbal and nonverbal communication.
Language Disorder is diagnosed when a person has ongoing difficulties learning language and communicating effectively with others, more so than peers their age. In turn, academic performance, emotional wellbeing, and relationships with others can be negatively affected.
Please visit the following sites for more information regarding Language Disorder:
https://www.asha.org/public/speech/disorders
https://www.cdc.gov/ncbddd/childdevelopment/language-disorders.html
https://childmind.org/guide/language-disorder
Book Recommendations:
The Parent’s Guide to Speech and Language Problems by Debbie Feit and Heidi M. Feldman
It Takes Two to Talk: A Practical Guide for Parents of Children with Language Delays by Elaine Weitzman and Jan Pepper
Childhood Speech, Language, and Listening Problems by Patricia McAleer Hamaguchi
Late-Talking Children: A Symptom or a Stage? by Stephen Camarata
Verbal speech requires putting together sounds to make words. Children learn some sounds early in development (/p/, /m/, or /w/), while learning other sounds are acquired later (/z/, /v/, or /th/). Almost all speech sounds, however, should be said correctly by age 4. Speech Sound Disorder is diagnosed when an individual is unable to create some or all of these sounds by the appropriate stage of development.
It is important to note that while articulation challenges can be perceived as “cute” during early childhood or assumed not to be a problem (“my child will grow out of it”), failure to receive the appropriate speech/language therapy early on can result in long-term speech difficulties that are far more resistant to intervention. Moreover, articulation challenges can result in your child being bullied by peers or feeling negatively about oneself.
Please visit the following sites for more information regarding Speech Sound Disorder:
https://www.asha.org/public/speech/disorders/Speech-Sound-Disorders
https://www.asha.org/Practice-Portal/Clinical-Topics/Articulation-and-Phonology
https://www.psychologytoday.com/us/conditions/speech-sound-disorder
https://childmind.org/guide/speech-sound-disorder
Book Recommendations:
The Parent’s Guide to Speech and Language Problems by Debbie Feit and Heidi M. Feldman
Childhood Speech, Language, and Listening Problems by Patricia McAleer Hamaguchi
Time to Talk: What You Need to Know About Your Child's Speech and Language Development by Michelle MacRoy-Higgins PhD, Carlyn Kolker
Interventions for Speech Sound Disorders in Children by A Lynn Williams and Sharynne McLeod and Rebecca J McCauley
Childhood-Onset Fluency Disorder is diagnosed when an individual has difficulty with the flow and timing of their speech pattern (e.g., hesitations, long pauses, repetition of syllables or words, etc.). Challenges in this area can result in anxiety regarding participating in class, communicating with others, and giving speeches.
Please visit the following sites for more information regarding Childhood-Onset Fluency Disorder:
https://www.mayoclinic.org/diseases-conditions/stuttering/symptoms-causes/syc-20353572
https://www.psychologytoday.com/us/conditions/childhood-onset-fluency-disorder
https://www.nidcd.nih.gov/health/stuttering
Book Recommendations:
Stuttering and Your Child: Questions and Answers by Edward G. Conture, Richard F. Curlee, Hugo H. Gregory, et. Al
If Your Child Stutters: A Guide for Parents by Stanley Ainsworth and Jane Fraser
Early Childhood Stuttering: Information and Support for Parents by J. Scott Yaruss and Reardon-Reeves
Minimizing Bullying for Children Who Stutter: A Practical Guide for SLPs by Nina Reardon-Reeves and J. Scott Yaruss
Social (Pragmatic) Communication Disorder is diagnosed when individuals struggle with the everyday social rules of communication (verbal and nonverbal), such as changing how they communicate in different situations (e.g., speaking in a library vs. a party) or for different audiences (e.g., peers vs. parents), following the rules of conversation (e.g., taking turns, using gestures, making eye contact, etc.), perspective taking (e.g., putting themselves in the shoes of others), and understanding norms.
Please visit the following sites for more information regarding Social (Pragmatic) Communication Disorder:
https://psychcentral.com/disorders/social-pragmatic-communication-disorder
https://www.asha.org/Practice-Portal/Clinical-Topics/Social-Communication-Disorders
https://childmind.org/guide/social-communication-disorder
Book Recommendations:
Quirky Kids: Understanding and Helping Your Child Who Doesn't Fit In- When to Worry and When Not to Worry by Eileen Costello and Perri Klass
Getting the Picture: Inference and Narrative Skills for Young People with Communication Difficulties by David Nash
Beyond Words: Using Paralanguage to Communicate Effectively by Pat Crissey
More Than Words: A Parent's Guide to Building Interaction and Language Skills for Children with Autism Spectrum Disorder or Social Communication Difficulties, 2nd Editionby Fern Sussman.
Autism Spectrum Disorder
Autism Spectrum Disorder is a developmental disorder that affects communication and behavior across school, work, and/or other areas of life. Although professionals can diagnose Autism Spectrum Disorder at any age, symptoms generally start to appear in early childhood. Importantly, while individuals with this diagnosis meet criteria for Social (Pragmatic) Communication Disorder, they also exhibit symptoms in the area(s) of restricted interests and/or repetitive behaviors.
Classification levels based on severity of symptoms:
| Severity Level | Social Communication | Restricted/Repetitive Behaviors | ||
|---|---|---|---|---|
| Level 1 “Requiring Support” | Without supports in place, deficits in social communication cause noticeable impairments. Difficulty initiating social interactions and clear examples of atypical or unsuccessful responses to social overtures of others. May appear to have decreased interest in social interactions. For example, a person who can speak in full sentences and engages in communication, but whose to-and-fro conversation with others fail and whose attempts to make friends are odd and possibly unsuccessful. | The inflexibility of behavior causes significant interference with functioning in one or more contexts—difficulty switching between activities. Problems of organization and planning hamper independence. | ||
| Level 2 “Requiring Substantial Support” | Marked deficits in verbal and nonverbal social communication skills; social impairments are apparent even with support in place; limited initiation of social interactions; and reduced or abnormal responses to social overtures from others. For example, a person who speaks simple sentences, whose interaction is limited to narrow special interests, and who has markedly odd nonverbal communication. | The inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors appears frequently enough to be obvious to the casual observer and interferes with functioning in various contexts. Distress and/or difficulty changing focus or action. | ||
| Level 3 “Requiring Very Substantial Support” | Severe deficits in verbal and nonverbal social communication skills cause severe impairments in functioning, very limited initiation of social interactions, and minimal response to social overtures from others. For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only straightforward strategies. | The inflexibility of behavior, extreme difficulty coping with change, or other restricted/repetitive behaviors markedly interfere with functioning in all spheres—great distress/difficulty changing focus or action. |
Please visit the following sites for more information regarding Autism Spectrum Disorder:
https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
https://www.cdc.gov/ncbddd/autism/facts.html
https://www.autismspeaks.org/what-autism
Video: Autism: One Man's Journey
https://www.elemy.com/studio/guides/parents-guide
https://www.elemy.com/studio/autism-resources/resources-and-help
https://www.elemy.com/studio/autism/levels
Research has shown that Autism Spectrum Disorder presents differently in females than males. Please visit the following sites for more information regarding the way Autism Spectrum Disorder presents in women:
https://www.healthline.com/health/autism-in-women
https://www.aane.org/women-asperger-profiles
https://www.autism.org.uk/about/what-is/gender/stories.aspx
https://childmind.org/article/autistic-girls-overlooked-undiagnosed-autism
Book Recommendations:
Parent/Caregivers:
A Practical Guide to Autism: What Every Parent, Family Member, and Teacher Needs to Know by Fred Volkmar and Lisa Wiesner
Getting the Best for Your Child with Autism: An Expert’s Guide to Treatment by Bryna Siegel
The Parent's Guide to College for Students on the Autism Spectrum by Lisa Med King and Lorraine E. Wolf
Girls Growing Up on the Autism Spectrum: What Parents and Professionals Should Know About the Pre-teen and Teenage Years by Shana Nichols
Autism-Asperger's and Sexuality: Puberty and Beyond by Jerry and Mary Newport
Asperger Syndrome and Adolescents, Helping Preteens and Teens Get Ready for the Real World by Teresa Bolick
The Breakaway: A Parent's Guide to Transitioning the Autistic and Twice Exceptional Adolescent Into Young Adulthood by Thomas W. Welch, Psy.D.
Younger Kids
All My Stripes: A Story for Children with Autism by Shaina Rudolph, Danielle Royer, and Jennifer Zivoin.
I am an Aspie Girl: A Book for Young Girls with Autism Spectrum Conditions by Danuta Bulhak-Paterson and Teresa Ferguson
It’s Perfectly Normal: Changing Bodies, Growing up, Sex & Sexual Health by Robie Harris and Michael Emberley
Boundaries: A Guide for Teens by Val Peter and Tom Dowd
A Smart Girl's Guide to Boys: Surviving Crushes, Staying True to Yourself, and Other Stuff (American Girl Library) by Nancy Holyoke
Adolescents
The Growing Up Guide for Girls: What Girls on the Autism Spectrum Need to Know! by Davida Hartman and Margaret Anne Suggs
The Asperkid's (Secret) Book of Social Rules: The Handbook of Not-So-Obvious Social Guidelines for Tweens and Teens with Asperger Syndrome by Jennifer Cook O'Toole.
College Students
Developing College Skills in Students with Autism and Asperger's Syndrome by Sarita Freedman
Realizing the College Dream with Autism or Asperger Syndrome by Ann Palmer
Students with Asperger Syndrome: A Guide for College Personnel by Lorraine E. Wolf
Girls, Women, and Non-Binary
Women and Girls with Autism Spectrum Disorder: Understanding Life Experiences from Early Childhood and Old Age by Jessica Kingley
Spectrum Women: Walking the Beat of Autism edited by Barb Book & Dr. Michelle Garnett
Six-Word Lessons on Female Asperger Syndrome: 100 Lessons to Understand and Support Girls and Women with Asperger’s (The Six-Word Lessons Series) by Tracey Cohen
The Growing Up Guide for Girls: What Girls on the Autism Spectrum Need to Know! by Davida Hartman
The Autism-Friendly Guide to Periods by Robyn Steward
Non-Binary
The Autistic Trans Guide to Life by by Yenn Purkis and Wenn B. Lawson
Autism Spectrum Disorder
Autism Spectrum Disorder is a developmental disorder that affects communication and behavior across school, work, and/or other areas of life. Although professionals can diagnose Autism Spectrum Disorder at any age, symptoms generally start to appear in early childhood. Importantly, while individuals with this diagnosis meet criteria for Social (Pragmatic) Communication Disorder, they also exhibit symptoms in the area(s) of restricted interests and/or repetitive behaviors.
Classification levels based on severity of symptoms:
| Level 1 “Requiring Support” (Social Communication) Without supports in place, deficits in social communication cause noticeable impairments. Difficulty initiating social interactions and clear examples of atypical or unsuccessful responses to social overtures of others. May appear to have decreased interest in social interactions. For example, a person who can speak in full sentences and engages in communication, but whose to-and-fro conversation with others fail and whose attempts to make friends are odd and possibly unsuccessful. | Level 1 “Requiring Support” (Restricted/Repetitive Behaviors) The inflexibility of behavior causes significant interference with functioning in one or more contexts—difficulty switching between activities. Problems of organization and planning hamper independence. |
| Level 2 “Requiring Substantial Support” (Social Communication) Marked deficits in verbal and nonverbal social communication skills; social impairments are apparent even with support in place; limited initiation of social interactions; and reduced or abnormal responses to social overtures from others. For example, a person who speaks simple sentences, whose interaction is limited to narrow special interests, and who has markedly odd nonverbal communication. | Level 2 “Requiring Substantial Support” (Restricted/Repetitive Behaviors) The inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors appears frequently enough to be obvious to the casual observer and interferes with functioning in various contexts. Distress and/or difficulty changing focus or action. |
| Level 3 “Requiring Very Substantial Support” (Social Communication) Severe deficits in verbal and nonverbal social communication skills cause severe impairments in functioning, very limited initiation of social interactions, and minimal response to social overtures from others. For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only straightforward strategies. | Level 3 “Requiring Very Substantial Support” (Restricted/Repetitive Behaviors) The inflexibility of behavior, extreme difficulty coping with change, or other restricted/repetitive behaviors markedly interfere with functioning in all spheres—great distress/difficulty changing focus or action. |
Please visit the following sites for more information regarding Autism Spectrum Disorder:
https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
https://www.cdc.gov/ncbddd/autism/facts.html
https://www.autismspeaks.org/what-autism
Video: Autism: One Man's Journey
https://www.elemy.com/studio/guides/parents-guide
https://www.elemy.com/studio/autism-resources/resources-and-help
https://www.elemy.com/studio/autism/levels
Research has shown that Autism Spectrum Disorder presents differently in females than males. Please visit the following sites for more information regarding the way Autism Spectrum Disorder presents in women:
https://www.healthline.com/health/autism-in-women
https://www.aane.org/women-asperger-profiles
https://www.autism.org.uk/about/what-is/gender/stories.aspx
https://childmind.org/article/autistic-girls-overlooked-undiagnosed-autism
Book Recommendations:
Parent/Caregivers:
A Practical Guide to Autism: What Every Parent, Family Member, and Teacher Needs to Know by Fred Volkmar and Lisa Wiesner
Getting the Best for Your Child with Autism: An Expert’s Guide to Treatment by Bryna Siegel
The Parent's Guide to College for Students on the Autism Spectrum by Lisa Med King and Lorraine E. Wolf
Girls Growing Up on the Autism Spectrum: What Parents and Professionals Should Know About the Pre-teen and Teenage Years by Shana Nichols
Autism-Asperger's and Sexuality: Puberty and Beyond by Jerry and Mary Newport
Asperger Syndrome and Adolescents, Helping Preteens and Teens Get Ready for the Real World by Teresa Bolick
The Breakaway: A Parent's Guide to Transitioning the Autistic and Twice Exceptional Adolescent Into Young Adulthood by Thomas W. Welch, Psy.D.
Younger Kids
All My Stripes: A Story for Children with Autism by Shaina Rudolph, Danielle Royer, and Jennifer Zivoin.
I am an Aspie Girl: A Book for Young Girls with Autism Spectrum Conditions by Danuta Bulhak-Paterson and Teresa Ferguson
It’s Perfectly Normal: Changing Bodies, Growing up, Sex & Sexual Health by Robie Harris and Michael Emberley
Boundaries: A Guide for Teens by Val Peter and Tom Dowd
A Smart Girl's Guide to Boys: Surviving Crushes, Staying True to Yourself, and Other Stuff (American Girl Library) by Nancy Holyoke
Adolescents
The Growing Up Guide for Girls: What Girls on the Autism Spectrum Need to Know! by Davida Hartman and Margaret Anne Suggs
The Asperkid's (Secret) Book of Social Rules: The Handbook of Not-So-Obvious Social Guidelines for Tweens and Teens with Asperger Syndrome by Jennifer Cook O'Toole.
College Students
Developing College Skills in Students with Autism and Asperger's Syndrome by Sarita Freedman
Realizing the College Dream with Autism or Asperger Syndrome by Ann Palmer
Students with Asperger Syndrome: A Guide for College Personnel by Lorraine E. Wolf
Girls and Women
Women and Girls with Autism Spectrum Disorder: Understanding Life Experiences from Early Childhood and Old Age by Jessica Kingley
Spectrum Women: Walking the Beat of Autism edited by Barb Book & Dr. Michelle Garnett
Six-Word Lessons on Female Asperger Syndrome: 100 Lessons to Understand and Support Girls and Women with Asperger’s (The Six-Word Lessons Series) by Tracey Cohen
The Growing Up Guide for Girls: What Girls on the Autism Spectrum Need to Know! by Davida Hartman
The Autism-Friendly Guide to Periods by Robyn Steward
Non-Binary
The Autistic Trans Guide to Life by by Yenn Purkis and Wenn B. Lawson
Attention Deficit/Hyperactvity Disorder
Attention-Deficit/Hyperactivity Disorder (ADHD) is diagnosed when there are persistent issues with attention/focus that cannot be accounted for by something else (e.g., anxiety, trauma, another medical condition). Oftentimes, executive functioning challenges are also exhibited, such as difficulty with organizing, planning, and time management. Although not always present, some individuals also show fidgety behaviors, hyperactivity, and/or impulsivity.
It is important to note that all children exhibit the above symptoms from time to time. In those with ADHD, however, symptoms are noticeably greater than with peers their age and cause distress and/or problems at home, at school/work, or with friends. Given the wide range of symptoms, an individual with ADHD will fall into one of three diagnostic categories: Predominantly Inattentive, Predominantly Hyperactive, and Combined Presentation.
Please visit the following sites for more information regarding Attention-Deficit/Hyperactivity Disorder:
https://www.cdc.gov/ncbddd/adhd/index.html
https://add.org/college-students
Book Recommendations:
ADHD-H or ADHD-C (for parents/caregivers with younger children)
Taking Charge of ADHD, 3rd Edition by Russell Barkley
Smart but Scattered: The Revolutionary "Executive Skills" Approach to Helping Kids Reach Their Potential by Peg Dawson and Richard Guare.
ADHD-I (for parents/caregivers with younger children)
Driven to Distraction (Revised): Recognizing and Coping with Attention Deficit Disorder by Edward Hallowell and John Ratey
Smart but Scattered: The Revolutionary "Executive Skills" Approach to Helping Kids Reach Their Potential by Peg Dawson and Richard Guare.
ADHD-H or ADHD-C (for parents/caregivers with teens)
Taking Charge of ADHD, 3rd Edition by Russell Barkley
Smart but Scattered Teens: The "Executive Skills" Program for Helping Teens Reach Their Potential by Peg Dawson and Richard Guare.
ADHD-I (for parents/caregivers with teens)
Driven to Distraction (Revised): Recognizing and Coping with Attention Deficit Disorder by Edward Hallowell and John Ratey
Smart but Scattered Teens: The "Executive Skills" Program for Helping Teens Reach Their Potential by Peg Dawson and Richard Guare.
ADHD for college students
Smart but Scattered--and Stalled: 10 Steps to Help Young Adults Use Their Executive Skills to Set Goals, Make a Plan, and Successfully Leave the Nest by Richard Guare, Colin Guare, and Peg Dawson.
On Your Own: A College Readiness Guide for Teens With ADHD/LD by Patricia Quinn and Theresa Maitland.
Specific Learning Disorders
Professionals diagnose a Specific Learning Disorder when an individual demonstrates difficulties in one or more foundational areas of academics that persistent despite intervention. When mild, or when an individual has strong compensatory strategies, a learning disability may not be recognized until late adolescence or adulthood. Within the above context, there are three types of Specific Learning Disorders, as indicated in greater detail below.
People with Specific Learning Disorder (SLD) with Impairment in Reading have difficulty connecting visual letters they see with the sounds they make in spoken words. In turn, this causes reading to be slow, effortful, and non-fluent. While many refer to Specific Learning Disorder with Impairment in Reading as “dyslexia,” this colloquial term is reserved for individuals with deficits in both reading fluency and decoding, rather than one or the other.
Please visit the following sites for more information regarding Specific Learning Disorder with Impairment in Reading:
https://childmind.org/article/understanding-dyslexia
Book Recommendations:
Straight Talk about Reading: How Parents Can Make a Difference during the Early Years by Susan Hall, Louisa Moats, and Lora Myers
Overcoming Dyslexia: A New and Complete Science-Based Program for Reading Problems at Any Level by Sally Shaywitz
All About IEPs: Answers to Frequently Asked Questions About IEPs by Peter Wright et al.
Specific Learning Disorder (SLD) with Impairment in Written Expression is diagnosed when there are persistent difficulties in the areas of spelling, grammar, punctuation, and/or written expression organization/clarity.
Please visit the following sites for more information regarding Specific Learning Disorder with Impairment in Written Expression:
http://ldanl.ca/resources/learning-disability-with-impairment-in-written-expression
Book Recommendations:
Dysgraphia: More than Just Bad Handwriting, A Parent's Perspective by J.S. Parent
Handwriting Brain-Body DisConnect : Adaptive Teaching Techniques to Unlock a Child's Dysgraphia for the Classroom and at Home by Cheri L. Dotterer
The Dysgraphia Sourcebook: Everything You Need to Help Your Child by Ben Bryce and Bill Stephens
All About IEPs: Answers to Frequently Asked Questions About IEPs by Peter Wright et al.
Specific Learning Disorder with Impairment in Mathematics is diagnosed when an individual has difficulties in grasping number-related concepts or utilizing symbols and functions when performing calculations. This includes number sense, math fact memorization, calculations, math reasoning, and math problem-solving.
Please visit the following sites for more information regarding Specific Learning Disorder with Impairment in Mathematics:
http://ldanl.ca/resources/learning-disability-with-impairment-in-mathematics
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803013
https://childmind.org/article/how-to-help-kids-dyscalculia
Book Recommendations:
Why Is Math So Hard for Some Children? The Nature and Origins of Mathematical Learning Difficulties and Disabilities by Daniel Berch and Michele Mazzocco
The Dyscalculia Toolkit by Ronit Bird
The Dyscalculia Resource Book: Games and Puzzles for Ages 7 to 14 by Ronit Bird
Math Handbook for Students with Math Difficulties, Dyscalculia, Dyslexia Or ADHD: (Grades 1-7) by Helmy Faber
Dyscalculia: From Science to Education by Brian Butterworth
All About IEPs: Answers to Frequently Asked Questions About IEPs by Peter Wright et al.
Nonverbal Learning Disorder
Professionals use the term Nonverbal Learning Disorder (or “a cluster of right hemispheric deficits”) when they observe an individual struggling with several right-hemispheric functions, such as understanding patterns, relationships, ideas, concepts, mathematics, and fine motor abilities. Nonverbal Learning Disorder is <strong>not</strong> an official diagnosis and is instead denoted under the diagnostic heading of Unspecified Neurodevelopmental Disorder or Other Specified Neurodevelopmental Disorder.
Children with NLD show weakness in one or more of the following five areas. It is important to note that not all children have gaps in all areas.
-
-
-
- Visual and Spatial Awareness
- Higher-Order Comprehension
- Social Communication
- Math Concepts
- Executive Functions
-
-
To learn more about Nonverbal Learning Disorder, please visit the following sites:
https://childmind.org/article/what-is-non-verbal-learning-disorder
https://www.psychologytoday.com/us/conditions/nonverbal-learning-disorder
https://ldaamerica.org/types-of-learning-disabilities/non-verbal-learning-disabilities
http://www.ldonline.org/article/6114
Book Recommendations:
Raising NLD Superstars: What Families with Nonverbal Learning Disabilities Need to Know About Nurturing Confident, Competent Kids by Marcia Brown Rubinstien
Nonverbal Learning Disabilities at Home: A Parent's Guide by Pamela B. Tanguay
Bridging the Gap: Raising a Child with Nonverbal Learning Disorder by Rondalyn Varney Whitney
NLD from the Inside Out: Talking to Parents, Teachers, and Teens about Growing Up with Nonverbal Learning Disabilities - Third Edition by Michael Brian Murphy
Helping Children with Nonverbal Learning Disabilities to Flourish: A Guide for Parents and Professionals by Marilyn Martin
Movement Disorders
Movement Disorders are a set of diagnoses that are characterized by deficits in fine motor (i.e., coordination between small muscles, like those of the hands and fingers) and/or gross motor (i.e., involve movements of the large muscles of the arms, legs, and torso) functions. Some examples include involuntary movement (e.g., tremor or spasms), abnormal posture, slowness, walking difficulty, and stiffness.
Professionals diagnose Developmental Coordination Disorder when they observe challenges with motor skills and coordination. Children with Developmental Coordination Disorder struggle with physical tasks and activities across settings, which can be particularly problematic in school (writing, copying from the board, and organizing their belongings).
Please visit the following sites for more information regarding Developmental Coordination Disorder:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1847727
https://childmind.org/article/problems-coordination-dyspraxia
https://www.psychologytoday.com/us/conditions/developmental-coordination-disorder
Book Recommendations:
Developmental Coordination Disorder: Hints and Tips for the Activities of Daily Living by Morven F. Ball
Developmental Dyspraxia: Identification and Intervention: A Manual for Parents and Professionals by Madeleine Portwood
Children with Developmental Coordination Disorder: Strategies for Success by Cheryl Missiuna
How to Help a Clumsy Child: Strategies for Young Children with Developmental Motor Concerns by Lisa A. Kurtz
Professionals diagnose Stereotypic Movement Disorder when they observe an individual moving in repetitive, purposeless ways (e.g., hand waving, body rocking, and head banging). Of note, this diagnosis is only given if the repetitive movement distress the child and lead to deficiencies in daily functioning. It is also important to determine whether Autism Spectrum Disorder is a more appropriate diagnosis if social communication/interaction weaknesses are also present.
Please visit the following sites for more information regarding Stereotypic Movement Disorder:
https://www.psychologytoday.com/us/conditions/stereotypic-movement-disorder
https://medlineplus.gov/ency/article/001548.htm
Book Recommendations:
A Practical Approach to Movement Disorders by Hubert Fernandez, Andre Machado, and Pandya, Mayur.
A Parent's Guide to Developmental Delays: Recognizing and Coping with Missed Milestones in Speech, Movement, Learning, and Other Areas by Laurie Fivozinsky LeComer
Tic Disorders
Tics can sometimes be difficult to diagnose, as a person’s tics may change over time. Moreover, they tend to come and go, and can get worse when a person is stressed or anxious. Of note, there are both simple and complex tics:
Motor Tics: Tics involving movements
Simple Motor Tics: These only impact a single muscle group. Examples of simple motor tics include, but are not limited to, nose wrinkling, head twitching, eye blinking, lip biting, facial grimacing, and shoulder shrugging.
Complex Motor Tics: These involve more than one muscle group. Although they generally appear to be intentional, they are not. Examples include, but are not limited to, kicking, skipping, jumping, mimicking, and smelling objects.
Vocal Tics: Tics involving sounds
Simple Vocal Tics: These involve one simple sound. Examples of simple vocal tics include coughing, throat clearing, grunting, sniffing, barking, and hissing.
Complex Vocal Tics: These involve more meaningful speech (like words). Examples of complex vocal tics include repeated words and phrases, animal sounds, and yelling.
Tourette's Disorder is a problem with the nervous system that results in an individual making sudden movements or sounds (tics) that cannot be controlled. For example, someone with Tourette's Disorder might blink or repeatedly clear their throat. Some blurt out unintentional words or phrases.
Please visit the following sites for more information regarding Tourette’s Disorder:
https://www.cdc.gov/ncbddd/tourette/diagnosis.html
https://tourette.org/about-tourette/overview/what-is-tourette
https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Tic-Disorders-035.aspx
https://childmind.org/guide/guide-to-chronic-motor-or-vocal-tic-disorder
https://crossword-solver.io/activities-for-people-with-tourette
Book Recommendations:
Calm and Control Vocal Tics and Bodily Twitches by Lynda Hudson
Tic Disorders: A Guide for Parents and Professionals by Uttom Chowdhury and Tara Murphy
Tourette Syndrome: Stop Your Tics by Learning What Triggers Them by Sheila Rogers Demare
Provisional Tic Disorder is the most common type of tic disorder. For this diagnosis to be made, the tics have been happening for less than a year.
Please visit the following sites for more information regarding Provisional Tic Disorder:
https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Tic-Disorders-035.aspx
https://childmind.org/guide/guide-to-chronic-motor-or-vocal-tic-disorder
Book Recommendations:
Calm and Control Vocal Tics and Bodily Twitches by Lynda Hudson
Tic Disorders: A Guide for Parents and Professionals by Uttom Chowdhury and Tara Murphy
Professionals diagnose Persistent (Chronic) Tic Disorder when an individual experiences tics for more than a year. Of note, tics may be motor or vocal, but not both, and they must have been occurring for at least a year.
Please visit the following sites for more information regarding Persistent (Chronic) Motor or Vocal Tic Disorder:
https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Tic-Disorders-035.aspx
https://childmind.org/guide/guide-to-chronic-motor-or-vocal-tic-disorder
Book Recommendations:
Calm and Control Vocal Tics and Bodily Twitches by Lynda Hudson
Tic Disorders: A Guide for Parents and Professionals by Uttom Chowdhury and Tara Murphy
Professionals diagnose a Tic Disorder when an individual persistently struggles with making an uncontrolled, sudden, repetitive movement or sound that is difficult to control. While Tic Disorders technically fall under the Movement Disorder classification (as seen above), it is important to highlight that Tic Disorders can include both movements and vocalizations. Therefore, for purposes of presenting information in an easy-to-understand format, we have dedicated an entire section to Tic Disorder.
Other Specified/Unspecified Neurodevelopmental Disorder
The most common “Other Specified Neurodevelopmental Disorder” is Neurodevelopmental Disorder Associated with (Medical Condition). This category applies to cases in which symptoms characteristic of a neurodevelopmental disorder are present and there is a known congenital medical condition (meaning the person was born with it) that has caused the neurodevelopmental disorder. Examples include, but are not limited to:
-
-
-
- Neurodevelopmental Disorder Associated with Teratogen Exposure to Cocaine
- Neurodevelopmental Disorder Associated with Preterm Birth and Low Birth Weight
-
-
Internet Resources:
Resources vary based on the medical condition and individual weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition and individual weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
This category applies to cases in which symptoms characteristic of a neurodevelopmental disorder are present, but there is no known etiology (i.e., medical condition) that has contributed.
Internet Resources:
Resources vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the observed weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
The diagnoses of Other Specified Neurodevelopmental Disorder and Unspecified Neurodevelopmental Disorder are clinically indicated when a person exhibits characteristics of a neurodevelopmental disorder, but their presentation is complicated. Reasons for this may be that the individual either does not meet full criteria for one or more of the above diagnoses or full criteria are met, but there is a known congenital medical etiology (i.e., the person was born with it) that has caused the neurodevelopmental disorder.
Neurocognitive Disorders
Neurocognitive Disorders are a group of diagnoses that account for decreased mental functioning as a result of a medical condition or event that occurred after birth. Symptoms vary in level of severity from mild to severe in terms of the level of impairment experienced.
Major or Mild Neurocognitive Disorder due to (a medical condition)
Neurocognitive Disorders are characterized by decreased mental function due to a medical condition or event other than a psychiatric illness. Professionals diagnose Major or Mild Neurocognitive Disorder due to [a medical condition] using medical history, physical examinations, and/or laboratory results.
Neurocognitive Disorders vary in level of severity:
Mild Neurocognitive Disorder: Difficulties are experienced only with complex daily activities like housework and money management.
Major Neurocognitive Disorder: The person is fully dependent on others for all activities.
Examples of medical conditions resulting in a neurocognitive disorder include:
-
-
-
- Alzheimer’s Disease
- Frontotemporal Lobar Degeneration
- Lewy Body Disease
- Vascular Disease
- Traumatic Brain Injury
- HIV Infection
- Prion Disease
- Parkinson’s Disease
- Huntington’s Disease
- Substance/medication use
- Another medical condition (examples include, but are not limited to, the following):
-
- Structural lesions (e.g. – primary or secondary brain tumors, subdural hematoma, slowly progressive or normal-pressure hydrocephalus)
- Hypoxia related to hypoperfusion from heart failure
- Endocrine conditions (e.g., hypothyroidism, hypercalcemia, hypoglycemia)
- Nutritional conditions (e.g., deficiencies of thiamine or niacin)
- Other infectious conditions (e.g., neurosyphilis, cryptococcosis)
- Immune disorders (e.g., temporal arteritis, systemic lupus erythematosus)
- Hepatic or renal failure, metabolic conditions (e.g., Kufs’ disease, adrenoleukodystrophy, metachromatic leukodystrophy, other storage diseases of adulthood and childhood)
- Other neurological conditions (e.g., epilepsy, multiple sclerosis)
- Unusual causes of central nervous system injury, such as electrical shock or intracranial radiation, are generally evident from the history
-
-
-
Internet Resources:
Resources vary based on the medical condition/event and individual weaknesses. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition/event and individual weaknesses. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Traumatic Brain Injury
A Traumatic Brain Injury (TBI) occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. While TBI is classified as “Neurocognitive Disorder due to a Traumatic Brain Injury,” it is important to highlight this diagnosis separately for educational purposes since it is common in the pediatric population.
Symptoms of a TBI can be mild, moderate, or severe, depending on the extent of the damage to the brain.
Mild: When suffering a mild Traumatic Brain Injury (mTBI), the individual may remain conscious or lose consciousness, but only for a few seconds or minutes. Following the injury, the individual may experience headaches, confusion, lightheadedness, dizziness, ringing in the ears, an unusual taste in their mouth, fatigue or lethargy, sleep changes, behavioral and mood changes, and/or difficulty with attention, memory, and concentration.
A person with a mild TBI may remain conscious or may experience a loss of consciousness for a few seconds or minutes. Other symptoms of mild TBI include headache, confusion, lightheadedness, dizziness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, a change in sleep patterns, behavioral or mood changes, and trouble with memory, concentration, attention, or thinking.
Moderate to Severe TBI: Individuals who have suffered a moderate or severe TBI exhibit many of the same symptoms as those with a mTBI, but at a greater intensity. The headache may get worse or not go away. An individual may repeatedly vomit or convulse. It may be very difficult or impossible to awaken them. They may exhibit slurred speech, numb or weak extremities, coordination difficulties, and increased confusion, restlessness, or agitation.
The following guidelines are used to determine the level of severity:
| Injury Characteristics | Mild TBI | Moderate TBI | Severe TBI | |
|---|---|---|---|---|
| Loss of consciousness | <30 min | 30 minutes to 24 hours | >24 hours | |
| Posttraumatic amnesia | <24 hours | 24 hours to 7 days | >7 days | |
| Disorientation and confusion at initial assessment (Glasgow Coma Scale) | A score of 13 to 15 (not below 13 at 30 minutes) | A score of 9 to 12 | A score of 3 to 8 |
Please visit the following sites for more information regarding Traumatic Brain Injury:
https://www.ninds.nih.gov/Disorders/All-Disorders/Traumatic-Brain-Injury-Information-Page
https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
https://www.cdc.gov/traumaticbraininjury/index.html
https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Traumatic-Brain-Injury
Book Recommendations:
The Brain Injury Workbook: Exercises for Cognitive Rehabilitation 2nd Edition by Trevor Powell
A Guided Meditation For Traumatic Brain Injury (TBI) by Belleruth Naparstek
Students with Brain Injury: Challenges for Identification, Learning, and Behavior In The Classroom by Katherine Kimes, Marilyn Lash, and Ronald Savage
Pediatric Traumatic Brain Injury: Proactive Intervention by Jean Blosser and Roberta DePompei
Traumatic Brain Injury
A Traumatic Brain Injury (TBI) occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. While TBI is classified as “Neurocognitive Disorder due to a Traumatic Brain Injury,” it is important to highlight this diagnosis separately for educational purposes since it is common in the pediatric population.
Symptoms of a TBI can be mild, moderate, or severe, depending on the extent of the damage to the brain.
Mild: When suffering a mild Traumatic Brain Injury (mTBI), the individual may remain conscious or lose consciousness, but only for a few seconds or minutes. Following the injury, the individual may experience headaches, confusion, lightheadedness, dizziness, ringing in the ears, an unusual taste in their mouth, fatigue or lethargy, sleep changes, behavioral and mood changes, and/or difficulty with attention, memory, and concentration.
A person with a mild TBI may remain conscious or may experience a loss of consciousness for a few seconds or minutes. Other symptoms of mild TBI include headache, confusion, lightheadedness, dizziness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, a change in sleep patterns, behavioral or mood changes, and trouble with memory, concentration, attention, or thinking.
Moderate to Severe TBI: Individuals who have suffered a moderate or severe TBI exhibit many of the same symptoms as those with a mTBI, but at a greater intensity. The headache may get worse or not go away. An individual may repeatedly vomit or convulse. It may be very difficult or impossible to awaken them. They may exhibit slurred speech, numb or weak extremities, coordination difficulties, and increased confusion, restlessness, or agitation.
The following guidelines are used to determine the level of severity:
| Injury Characteristics Loss of consciousness | Mild TBI <30 min | Moderate TBI 30 minutes to 24 hours | Severe TBI >24 hours |
| Injury Characteristics Posttraumatic amnesia | Mild TBI <24 hours | Moderate TBI 24 hours to 7 days | Severe TBI >7 days |
| Injury Characteristics Disorientation and confusion at initial assessment (Glasgow Coma Scale) | Mild TBI A score of 13 to 15 (not below 13 at 30 minutes) | Moderate TBI A score of 9 to 12 | Severe TBI A score of 3 to 8 |
Please visit the following sites for more information regarding Traumatic Brain Injury:
https://www.ninds.nih.gov/Disorders/All-Disorders/Traumatic-Brain-Injury-Information-Page
https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
https://www.cdc.gov/traumaticbraininjury/index.html
https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Traumatic-Brain-Injury
Book Recommendations:
The Brain Injury Workbook: Exercises for Cognitive Rehabilitation 2nd Edition by Trevor Powell
A Guided Meditation For Traumatic Brain Injury (TBI) by Belleruth Naparstek
Students with Brain Injury: Challenges for Identification, Learning, and Behavior In The Classroom by Katherine Kimes, Marilyn Lash, and Ronald Savage
Pediatric Traumatic Brain Injury: Proactive Intervention by Jean Blosser and Roberta DePompei
Mental Health Disorders
According to the National Alliance on Mental Illness (NAMI): “A mental illness is a condition that affects a person’s thinking, feeling, behavior or mood. These conditions deeply impact day-to-day living and may also affect the ability to relate to others. If you have — or think you might have — a mental illness, the first thing you must know is that you are not alone. Mental health conditions are far more common than you think, mainly because people do not like to, or are scared to, talk about them.” Read more from NAMI on Mental Illness:
Read More- 1 in 5 adults experience mental illness each year
- 1 in 25 adults experience serious mental illness each year
- 1 in 6 youth aged 6-17 experience a mental health disorder each year
- 50%of all lifetime mental illness begins by age 14, and 75% by age 24
“A mental health condition is not the result of one thing. Research suggests multiple, linking causes. Genetics, environment, and lifestyle influence whether someone develops a mental health condition. A stressful job or home life makes some people more susceptible to traumatic life events. Biochemical processes and circuits and basic brain structure may play a role, too.
None of this means that you are broken or that you, or your family, did something “wrong.” Mental illness is no one’s fault. And for many people, recovery — including meaningful roles in social life, school, and work — is possible, especially when you start treatment early and play a strong role in your own recovery process.”
Bipolar Disorders
Bipolar Disorders are a set of diagnoses that causes unusual shifts in mood, energy, activity level, and concentration, which make it difficult to engage in daily tasks. Moods typically vacillate between periods of “highs,” such as feeling elated, irritable, or energized (known as manic episodes) to periods of “lows,” such as feelings of sadness, indifference, or hopelessness (known as depressive episodes). Less severe manic periods are known as hypomanic episodes.
Examples of mania and hypomania area generally the same, but vary in their degree of severity:
-
-
-
- Higher-than-normal energy levels
- Restlessness or inability to sit still
- Decreased need for sleep
- Increased self-esteem or confidence, or grandiosity
- Extremely talkative
- Racing thoughts
- New ideas and plans
- Easily distracted
- Taking on multiple projects with no way of finishing them
- Decreased inhibitions
- Increased sexual desire
- Engaging in risky behavior, such as having impulsive sex, gambling with life savings, or going on big spending sprees
-
-
Bipolar I Disorder is diagnosed when there is a distinct period (one week or longer) of manic symptoms so pronounced that the person may require hospital care. Depressive episodes also occur and last for a minimum of two weeks. Periods of mixed features (manic and depressive symptoms) can also occur.
Bipolar II Disorder is diagnosed when there is a pattern of depressive and hypomanic symptoms without mania. There must be one or more major depressive episode and at least one hypomania episode. The hypomanic episode must last for most of the day each day for at least four days.
Please visit the following sites for more information regarding Bipolar I and Bipolar II Disorder:
https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Bipolar-Disorder
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955
https://www.drugwatch.com/health/mental-health/mental-illness/bipolar-disorder
Book Recommendations:
The Bipolar Teen: What You Can Do to Help Your Child and Your Family by David J. Miklowitz and Elizabeth Levergood George
What Works for Bipolar Kids: Help and Hope for Parents by Mani N. Pavuluri
If Your Adolescent Has Depression Or Bipolar Disorder: An Essential Resource for Parents by Dwight L. Evans and Linda Wasmer Andrews
The Everything Parent's Guide To Children With Bipolar Disorder: Professional, Reassuring Advice to Help You Understand And Cope by Jeffery Naser and William Stillman
Raising a Moody Child: How to Cope with Depression and Bipolar Disorder by Jill S. Goldberg Arnold and Mary Fristad
The Bipolar Disorder Survival Guide, Third Edition: What You and Your Family Need to Know 3rd Edition by David Miklowitz
Cyclothymic Disorder (Cyclothymia) is a form of Bipolar Disorder characterized by distinct periods of hypomania (elevated mood) and depressive symptoms experienced for two years or longer. However, mood fluctuations are not sufficient in number, severity, or duration to meet the full criteria for a hypomanic or depressive episode. For Cyclothymic Disorder to be diagnosed, symptoms must be present for at least half the time and do not disappear for more than two months at any time.
Please visit the following sites for more information about Cyclothymic Disorder:
https://www.psychologytoday.com/us/conditions/cyclothymic-disorder
https://www.mayoclinic.org/diseases-conditions/cyclothymia/symptoms-causes/syc-20371275
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3609426
https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Bipolar-Disorder
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955
Book Recommendations:
The Bipolar Teen: What You Can Do to Help Your Child and Your Family by David J. Miklowitz and Elizabeth Levergood George
What Works for Bipolar Kids: Help and Hope for Parents by Mani N. Pavuluri
If Your Adolescent Has Depression Or Bipolar Disorder: An Essential Resource for Parents by Dwight L. Evans and Linda Wasmer Andrews
The Everything Parent's Guide To Children With Bipolar Disorder: Professional, Reassuring Advice to Help You Understand And Cope by Jeffery Naser and William Stillman
Raising a Moody Child: How to Cope with Depression and Bipolar Disorder by Jill S. Goldberg Arnold and Mary Fristad
The Bipolar Disorder Survival Guide, Third Edition: What You and Your Family Need to Know 3rd Edition by David Miklowitz
Professionals diagnose Substance/Medication-Induced Bipolar and Related Disorder when a substance or medication directly induces mania, hypomania, or a major depressive episode.
Internet Resources:
Resources vary based on the substance(s) used. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the substance(s) used. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Professionals diagnose Bipolar and Related Condition Due to Another Medical Condition when an individual experiences periods of mania/hypomania and depression directly as a result of a medical condition.
Internet Resources:
Resources vary based on the medical condition. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Depressive Disorders
Depressive Disorders are a set of diagnoses characterized by persistent feelings of sadness and worthlessness, as well as a lack of desire to engage in formerly pleasurable activities. All people experience brief periods of a “down” mood. However, true depression is more severe and persistent. It is a very serious condition that can negatively affect sleep, energy levels, appetite, information processing, and interpretation of experiences. Professionals can treat depression with psychotherapy, medication, or a combination of both (most effective).
Professionals diagnose Disruptive Mood Dysregulation Disorder when they observe severe and frequent temper outbursts that affect one’s ability to function at home, in school, and with their friends. Many children express irritability, upset, or moodiness from time to time. However, unusually significant and/or persistent expressions may point to Disruptive Mood Dysregulation Disorder.
Please visit the following sites for more information regarding Disruptive Mood Dysregulation Disorder:
https://childmind.org/guide/guide-to-disruptive-mood-dysregulation-disorder
https://psychcentral.com/disorders/disruptive-mood-dysregulation-disorder
https://www.psychologytoday.com/us/conditions/depressive-disorders
Book Recommendations:
1-2-3 Magic: 3-Step Discipline for Calm, Effective, Happy Parenting by Thomas Phelan
SOS: Help for Parents, 3rd Edition by Lynn Clark, Your Defiant Child, 2nd Edition: Eight Steps to Better Behavior by Christine M. Benton and Russell Barkley
The Explosive Child by Ross Greene.
Major Depressive Disorder is diagnosed when an individual experiences chronic sadness, feelings of worthlessness, irritability, lethargy, sleep disruptions, appetite disturbances, and sometimes even thoughts of death. While everyone feels sad or down from time to time, Major Depressive Disorder extends far beyond normal unhappiness. Moreover, the persistence of a sad or irritable mood affects an individual’s thinking and behavior across settings, such as at home, in school, and with friends. Early and consistent treatment reduces the severity of symptoms and decreases the risk of recurrence, while improving functioning and overall well-being.
Please visit the following sites for more information regarding Major Depressive Disorder:
https://childmind.org/guide/major-depressive-disorder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6213890
https://www.chop.edu/conditions-diseases/major-depression-children
https://www.stanfordchildrens.org/en/topic/default?id=major-depression-in-children-90-P02569
https://www.stanfordchildrens.org/en/topic/default?id=major-depression-in-adolescents-90-P01614
https://www.parentbooks.ca/Depression_Resources_for_Kids_&_Teens.html
https://www.intelligent.com/online-college-guide-for-students-with-mental-health-disorders
Book Recommendations:
Battling the Blues: the Handbook for Helping Children and Teens with Depression by Kim “Tip” Frank
Beyond the Blues: Child and Youth Depression by Helen Slinger and Maureen Palmer
Beyond the Blues: A Workbook for Teens Who Are Depressed by Lisa Schab
Blueloon by Julia Cook
Can I Tell You about Depression? A Guide for Friends, Family and Professionals by Christopher Dowrick and Susan Martin
Conquer Negative Thinking for Teens: A Workbook to Break the Nine Thought Habits That Are Holding You Back by Mary Karapetian Alvord and Anne McGrath
Coping with An Anxious or Depressed Child by Samantha Cartwright-Hatto
Professionals diagnose Persistent Depressive Disorder (Dysthymia) when an individual continuously suffers from depression. Symptoms include hopelessness, productivity issues, low self-esteem, and a loss of interest in previously enjoyed activities, often over years.
Please visit the following sites for more information regarding Persistent Depressive Disorder:
https://childmind.org/guide/persistent-depressive-disorder-dysthymia
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P01600
https://www.intelligent.com/online-college-guide-for-students-with-mental-health-disorders
Book Recommendations:
Battling the Blues: the Handbook for Helping Children and Teens with Depression by Kim “Tip” Frank
Beyond the Blues: Child and Youth Depression by Helen Slinger and Maureen Palmer
Beyond the Blues: A Workbook for Teens Who Are Depressed by Lisa Schab
Blueloon by Julia Cook
Can I Tell You about Depression? A Guide for Friends, Family and Professionals by Christopher Dowrick and Susan Martin
Conquer Negative Thinking for Teens: A Workbook to Break the Nine Thought Habits That Are Holding You Back by Mary Karapetian Alvord and Anne McGrath
Coping with An Anxious or Depressed Child by Samantha Cartwright-Hatto
Professionals diagnose Depressive Disorder Due To Another Medical Condition when a certain medical condition results in depression that otherwise would not be present. DSM-5. One example is hypothyroidism.
Internet Resources:
Resources vary based on the medical condition. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Anxiety Disorders
Occasional anxiety is an expected part of life. Your child might feel anxious when faced with a problem at school, before taking a test, or before making an important decision. Anxiety Disorders, however, involve more than temporary worry or fear. For a person with an Anxiety Disorder, these feelings do not just go away. Moreover, worries or fears can get worse over time and can interfere with daily activities, such as schoolwork, family time, playing with peers, etc.
Professionals diagnose Separation Anxiety Disorder when an individual exhibits persistent fears about being away from loved ones or that something awful will happen to a loved one. Separation anxiety is typical in young children, but should slowly taper off as one enters elementary school. If, however, significant symptoms are exhibited that interfere with daily activities (e.g., attending school, unwillingness to engage in social interactions with peers, etc.) or moderate levels of separation anxiety persist as one matures, a diagnosis of Social Anxiety Disorder may be clinically indicated.
Please visit the following sites for more information about Separation Anxiety Disorder:
https://www.stanfordchildrens.org/en/topic/default?id=separation-anxiety-disorder-90-P02582
https://childmind.org/guide/separation-anxiety-disorder
https://www.psychologytoday.com/us/conditions/separation-anxiety
https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
Book Recommendations:
Helping Your Child Overcome Separation Anxiety Or School Refusal: A Step-by-step Guide for Parents by Andrew R. Eisen and Linda B. Engler
Separation Anxiety in Children and Adolescents: An Individualized Approach to Assessment and Treatment by Andrew R. Eisen and Charles E. Schaefer
Freeing Your Child from Anxiety: Powerful, Practical Solutions to Overcome Your Child's Fears, Worries, and Phobias by Tamar Chansky
I Don't Want To Go To School: Helping Children Cope with Separation Anxiety by Nancy Pando
Helping Your Anxious Child: A Step-by-Step Guide for Parents 2nd Edition: A Step-By-Step Guide for Parents by Ronald Rapee, Ann Wignall, Susan Spence, Vanessa Cobham, and Heidi Lyneham
Selective Mutism is a complex childhood anxiety disorder demarcated by an inability to speak and communicate effectively in certain social settings, such as school. Individuals with Selective Mutism are, however, able to speak and communicate in settings where they are comfortable and feel safe. Nine out of ten children with Selective Mutism also suffer from social phobia/anxiety. These issues expand under any type of pressure.
Please visit the following sites for more information regarding Selective Mutism:
https://selectivemutismcenter.org/whatisselectivemutism
https://www.asha.org/public/speech/disorders/Selective-Mutism
https://www.selectivemutism.org
https://childmind.org/guide/selective-mutism
https://www.psychologytoday.com/us/conditions/selective-mutism
https://adaa.org/living-with-anxiety/children/selective-mutism
https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
Book Recommendations:
Can I Tell You about Selective Mutism? A Guide for Friends, Family and Professionals by Alison Wintgens and Maggie Johnson
Helping Your Child with Selective Mutism: Practical Steps to Overcome a Fear of Speaking by Angela E. McHolm, Charles E. Cunningham, and Melanie K. Vanier
Selective Mutism: An Assessment and Intervention Guide for Therapists, Educators & Parents by Aimee Kotrba
The Selective Mutism Treatment Guide: Manuals for Parents, Teachers, and Therapists by Ruth Perednik
Maya's Voice by Wen-Wen Cheng
Social Anxiety Disorder is diagnosed when an individual demonstrates extreme fear or anxiety regarding being judged by others. Typically, social anxiety manifests in a group or public setting, resulting in the individual feeling awkward, exposed, or negatively judged in some way. However, other individuals experience performance anxiety (e.g., test taking, competitions, performing a task in front of others) when they are overly concerned about how their actions will be judged by others, particularly those in authority. The above fears can sometimes lead to avoidance. Commonly, physical symptoms co-exist with social anxiety, such as sweating, nausea, a rapid heartbeat, and/or panic symptoms.
Please visit the following sites for more information regarding Social Anxiety Disorder:
https://adaa.org/understanding-anxiety/social-anxiety-disorder
https://www.mayoclinic.org/diseases-conditions/social-anxiety-disorder/symptoms-causes/syc-20353561
https://childmind.org/guide/social-anxiety-disorder
https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
Book Recommendations:
Helping Your Anxious Child: A Step-by-Step Guide for Parents 2nd Edition: A Step-By-Step Guide for Parents by Rondal Rapee, Ann Wignall, Susan Spence, Venssa Cobham, and Heidi Lyneham
Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child's Fears, Worries, and Phobias by Tamar Chansky
Overcoming Your Child's Shyness and Social Anxiety by Cathy Creswell and Lucy Willetts
Raising the Shy Child: A Parent's Guide to Social Anxiety by Christine Fonseca
Professionals diagnose Specific Phobia when an individual exhibits substantial anxiety in the presence of a certain object or situation, in turn leading to avoidance. The anxiety or fear is said to be “irrational” because the object or situation presents little or no actual danger.
Examples include:
Animal Phobias: Fear involves specific animals, such as mice, dogs, or insects. This is the most common phobia category.
Situational Phobias: Fear involve specific situations, such as riding in a car, traveling on a bus, flying in an airplane, or being stuck in a confined space.
Natural Environment Phobias: Fear involves any phobia related to nature, such as lightning, water, or a fear of heights.
Blood-Injection-Injury Phobias: Fear involves blood, injury, and standard medical procedures (e.g., shots, blood draws, surgical procedures).
Other Phobias: Fear involves anything that is not under the umbrella of the different forms of Specific Phobia, such as fireworks or circus performers.
Please visit the following sites for more information regarding Specific Phobias:
https://www.mayoclinic.org/diseases-conditions/specific-phobias/symptoms-causes/syc-20355156
https://adaa.org/understanding-anxiety/specific-phobias
https://adaa.org/understanding-anxiety/specific-phobias/symptoms
https://childmind.org/guide/specific-phobia
Book Recommendations:
Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child's Fears, Worries, and Phobias by Tamar Chansky
Beyond Anxiety and Phobia: A Step-by-Step Guide to Lifetime Recovery by Edmund J. Bourne
Monsters under the Bed and Other Childhood Fears: Helping Your Child Overcome Anxieties, Fears, and Phobias by Marianne Daniels Garber, Robyn Freedman Spizman, Stephen W. Garber
Lights Out!: Helping Your Kids Overcome Their Fear of the Dark by Chad Cramer
Why Your Child Is Afraid: Understanding the Normal Fears of Childhood from Birth to Adolescence and Helping Overcome Them by Robert Schachter
Panic Disorder is characterized by perpetual periods of extreme discomfort and fear that lasts for several minutes to hours. Physical symptoms often co-exist, such as sweating, nausea, rapid heartbeat, and vomiting. Episodes often take place without any warning.
Please visit the following sites for more information regarding Panic Disorder:
https://childmind.org/guide/panic-disorder
https://adaa.org/living-with-anxiety/children/childhood-anxiety-disorders
https://adaa.org/sites/default/files/Anxiety%20Disorders%20in%20Children.pdf
https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
Book Recommendations:
My Anxious Mind : A Teen's Guide to Managing Anxiety and Panic by Michael A. Tompkins and Katherine A. Martinez
Helping Your Anxious Child: A Step-by-Step Guide for Parents 2nd Edition: A Step-By-Step Guide for Parents by Rondal Rapee, Ann Wignall, Susan Spence, Venssa Cobham, and Heidi Lyneham
Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child's Fears, Worries, and Phobias by Tamar Chansky
Anxiety, Worry, OCD and Panic Attacks ‑ The Definitive Recovery Approach by Lauren Callaghan
School Phobia, Panic Attacks, and Anxiety in Children by Marianna Csoti
Agoraphobia is an anxiety disorder defined by symptoms of anxiety in situations where an individual perceives their environment to be unsafe with no easy way to escape, especially when alone. Examples include, but are not limited to:
-
-
-
- Buses, trains, or planes
- Open areas
- Enclosed areas
- Crowded areas
- Being outside the home alone
-
-
Please visit the following sites for more information regarding Agoraphobia:
https://childmind.org/article/agoraphobia-in-children
http://www.childrenshospital.org/conditions-and-treatments/conditions/p/phobias/symptoms-and-causes
https://www.psychologytoday.com/us/blog/suffer-the-children/201111/the-agoraphobic-girl
Book Recommendations:
Sometimes I Worry Too Much But Now I Know How to Stop Book: A Book to Help Children by Dawn Huebner
The Agoraphobia Workbook by C Alec Pollard and Elke Zuercher White
Helping Your Anxious Child: A Step-by-Step Guide for Parents 2nd Edition: A Step-By-Step Guide for Parents by Rondal Rapee, Ann Wignall, Susan Spence, Venssa Cobham, and Heidi Lyneham
Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child's Fears, Worries, and Phobias by Tamar Chansky
My Anxious Mind : A Teen's Guide to Managing Anxiety and Panic by Michael A. Tompkins and Katherine A. Martinez
Professionals diagnose Generalized Anxiety Disorder when an individual exhibits unnecessary and uncontrollable uneasiness, worries, and fears broad in nature and persistent throughout the day. The individual may also experience headaches, muscular pain, restlessness, increased heart rate, and stomachaches. Reassurance from others helps, but only for a brief time before anxiety arises again.
Please visit the following sites for more information regarding Generalized Anxiety Disorder:
https://childmind.org/guide/guide-to-generalized-anxiety-disorder
https://adaa.org/sites/default/files/Anxiety%20Disorders%20in%20Children.pdf
https://kidshealth.org/en/parents/anxiety-disorders.html
http://www.worrywisekids.org/node/24
https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml
https://www.intelligent.com/online-college-guide-for-students-with-mental-health-disorders
Book Recommendations:
A Kids Book About Anxiety by Ross Szabo
Freeing Your Child from Negative Thinking: Powerful, Practical Strategies to Build a Lifetime of Resilience, Flexibility, and Happiness by Tamar Chansky
Freeing Your Child from Anxiety by Tamar Chansky
Parenting the New Teen in the Age of Anxiety by John Duffy
Helping Your Anxious Child by Ronald Rapee, Ann Wignall, Susan Spencer, et al.
Professionals diagnose Anxiety Disorder Due to Another Medical Condition when they observe unnecessary and uncontrollable uneasiness in an individual following the onset, or persistence, of a medical condition. The individual may also experience headaches, muscular pain, restlessness, an increased heart rate, and stomachaches, leading to an enhanced and unreasonable fear of normal situations.
Internet Resources:
Resources vary based on the medical condition. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Obsessive-Compulsive and Related Disorders
There are several diagnoses that fall under the broad heading of Obsessive-Compulsive and Related Disorders, all of which share the commonality of obsessions and compulsions.
Obsessions: Continual and insistent thoughts, impulses, or images that are unpleasant and difficult to control.
Compulsions: Repeated behaviors that an individual feels compelled to perform, followed by a sense of relief.
Many individuals struggle with body-focused repetitive behaviors (e.g., hair pulling, skin picking, hand-washing), while others focus on external compulsions (e.g., rechecking locks, aligning toys or items, counting, repeating a task a certain number of times).
Professionals diagnose Obsessive-Compulsive Disorder when observing instances of both obsessions and compulsions in an individual that interfere with their quality of life and functionality.
Examples of Obsessions:
-
-
-
- Fear of germs or contamination
- Unwanted thoughts involving sex, religion, or harm
- Desiring symmetry or perfection
-
-
Examples of Compulsions:
-
-
-
- Excessive cleaning and/or hand washing
- Ordering and arranging things in a specific way
- Repeatedly checking things (e.g., door is locked or the oven is off)
- Compulsive counting
-
-
Individuals with Obsessive-Compulsive Disorder generally:
-
-
-
- Have significant difficulty controlling their thoughts/behaviors related to obsessions/compulsions
- Spend an hour or more per day on unwanted thoughts and behaviors
- Experience a fleeting sense of relief when engaging in the compulsion, but quickly feel anxious again
- Feel limited and unable to fully enjoy their lives because of these obsessions and compulsions
-
-
Please visit the following sites for more information regarding Obsessive-Compulsive Disorder:
https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
https://www.psychiatry.org/patients-families/ocd/what-is-obsessive-compulsive-disorder
Book Recommendations:
Talking Back to OCD: The Program That Helps Kids and Teens Say "No Way" -- and Parents Say "Way to Go" by John S. March
Freeing Your Child from Obsessive-Compulsive Disorder: A Powerful, Practical Program for Parents of Children and Adolescents by Tamar Chansky
Helping Your Child with OCD: A Workbook for Parents of Children with OCD by Cherry Pedrick and Lee Fitzgibbons
Up and Down the Worry Hill: A Children's Book about OCD by Aureen Pinto Wagner
What to Do When Your Brain Gets Stuck: A Kid's Guide to Overcoming OCD by Dawn Huebner
The OCD Workbook for Kids: Skills to Help Children Manage Obsessive Thoughts and Compulsive Behaviors by Anthony C. Puliafico and Joanna A. Robin
Body Dysmorphic Disorder is diagnosed when a person experiences uncontrollable thoughts about the way they feel regarding a perceived flaw regarding one or more of their body parts, which is generally imperceptible to others. In turn, there may be avoidance of otherwise pleasant social occasions out of fear and embarrassment. The individual may continually seek reassurance, look at themselves in the mirror, groom themselves obsessively, and/or take excessive photos of themselves.
Please visit the following sites for more information regarding Body Dysmorphic Disorder:
https://childmind.org/guide/guide-to-body-dysmorphic-disorder
https://www.mayoclinic.org/diseases-conditions/body-dysmorphic-disorder/symptoms-causes/syc-20353938
https://bdd.iocdf.org/about-bdd
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181960
Book Recommendations:
The Parents' Guide to Body Dysmorphic Disorder: How to Support Your Child, Teen or Young Adult by Nicole Schnackenberg and Amita JassiBenedetta Monzani
No Body's Perfect : Stories by Teens about Body Image, Self-Acceptance, and the Search for Identity by Kimberly Kirberger
The Body Image Survival Guide for Parents: Helping Toddlers, Tweens, and Teens Thriveby Marci Warhaft-Nadler
Healthy Teens Body and Soul: A Parent's Complete Guide by Andrea Marks and Betty Rothbart
Hoarding Disorder is characterized by a person acquiring objects in great excess and being unable or unwilling to part with them for any reason, including safety. These behaviors often resulting in strained relationships with others, as well as stressful, cluttered, and distracting environments. Any attempt by an outside party to remove some or all of the objects is typically met with anger and/or severe anxiety. There is also a pronounced preoccupation with these belongings.
Please visit the following sites for more information regarding Hoarding Disorder:
https://childmind.org/guide/hoarding-disorder
https://www.anxiety.org/is-your-child-a-hoarder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4558984
Book Recommendations:
From Hoarding to Hope: Understanding People Who Hoard and How to Help Them by Geralin Thomas
Trichotillomania is a disorder characterized by the urge to pull out one’s hair, whether it be from the scalp or other parts of the body (e.g., eyelashes, brows, genitals, back, arms, legs), sometimes followed by a sense of relief. However, some do it unconsciously.
Please visit the following sites for more information regarding Trichotillomania:
https://childmind.org/guide/trichotillomania
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4857813
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3366724
https://kidshealth.org/en/teens/trichotillomania.html
Book Recommendations:
A Parent Guide to Hair Pulling Disorder: Effective Parenting Strategies for Children with Trichotillomania by Ruth Goldfinger Golomb and Suzanne Mouton-Odum
Stay Out of My Hair! Parenting Your Child with Trichotillomania by Ruth Goldfinger Golomb and Suzanne Mouton-Odum
The Hair Pulling Habit and You: How to Solve the Trichotillomania Puzzle by Ruth Goldfinger Golomb and Sherrie Mansfield Vavrichek
Excoriation is a disorder characterized by recurrent skin picking resulting in open sores and/or scaring. While some individuals feel compelled to pick at their skin and then feel a sense of relief thereafter, other individuals do it unconsciously. Excoriation often leads to embarrassment and shame, especially when wounds or scaring are visible to others.
Please visit the following sites for more information regarding Excoriation:
https://childmind.org/guide/guide-to-excoriation
https://www.psychologytoday.com/us/conditions/dermatillomania-skin-picking
https://childadvocate.net/skin-picking-and-self-injurious-behavior
https://www.mhanational.org/conditions/excoriation-disorder-skin-picking-or-dermatillomania
Book Recommendations:
Stop Skin Picking: How to Break the Habit of Skin Picking and Effectively Cure Dermatillomania by Andrea Hart and Andrea Hart
Skin Picking: The Freedom to Finally Stop by Annette Pasternak
Professionals diagnose Obsessive-Compulsive and Related Disorder Due to Another Medical Condition when they observe obsessions and/or compulsions following the onset, or persistence, of a medical condition.
Internet Resources:
Resources vary based on the medical condition. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the medical condition. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Trauma- and Stressor-Related Disorders
Trauma and Stressor-Related Disorders are a set of diagnoses that are characterized by emotional and behavioral problems resulting from traumatic and stressful experiences, such as exposure to physical or emotional violence or pain.
Reactive Attachment Disorder is diagnosed when infants and young children subjected to extreme neglect or abuse fail to establish expected bonds with caregivers, which subsequently affects their ability to appropriately connect with others as they mature. An individual with this diagnosis does not seek comfort from caregivers and instead becoming distressed (e.g., irritable, angry, scared) or indifferent during their interactions.
Please visit the following sites for more information regarding Reactive Attachment Disorder:
https://childmind.org/guide/reactive-attachment-disorder
https://www.psychologytoday.com/us/conditions/reactive-attachment-disorder
Book Recommendations:
When Love Is Not Enough: A Guide to Parenting with RAD‑Reactive Attachment Disorder by Nancy L. Thomas
Parenting Pandora: Understanding Your Child With Reactive Attachment Disorder by Essie Johnson
You Are Not Alone: A Book of Hope for Parents Dealing with Reactive Attachment Disorder by Kate Silvas
Parenting the Hurt Child: Helping Adoptive Families Heal and Grow by Gregory C. Keckand Regina M. Kupecky
Integrative Parenting: Strategies for Raising Children Affected by Attachment Trauma by Cathy Schweitzer, Debra Wesselmann, and Stefanie Armstrong
Similar to Reactive Attachment Disorder, Disinhibited Social Engagement Disorder is diagnosed when infants and young children subjected to extreme neglect or abuse fail to establish expected bonds with caregivers, which subsequently affects their ability to appropriately connect with others as they mature. However, unlike Reactive Attachment Disorder, those with Disinhibited Social Engagement Disorder will attempt to become overly attached to others very quickly and in an inappropriate fashion that violates cultural norms.
Please visit the following sites for more information regarding Disinhibited Social Engagement Disorder:
https://www.psychologytoday.com/us/conditions/disinhibited-social-engagement-disorder
https://www.healthline.com/health/disinhibited-social-engagement-disorder
https://www.verywellmind.com/what-is-disinhibited-social-engagement-disorder-4138254
Book Recommendations:
Integrative Parenting: Strategies for Raising Children Affected by Attachment Trauma by Cathy Schweitzer, Debra Wesselmann, and Stefanie Armstrong
Parenting the Hurt Child: Helping Adoptive Families Heal and Grow by Gregory C. Keckand Regina M. Kupecky
Posttraumatic-Stress Disorder is diagnosed when an individual is exposed to a life-threatening event (either personally or observed) and continues to exhibit trauma-related symptoms (e.g., flashbacks, nightmares, avoidance, difficulty concentrating and engaging in daily activities, withdrawal, etc.) for more than one month after the incident.
Please visit the following sites for more information regarding Posttraumatic-Stress Disorder:
https://www.cdc.gov/childrensmentalhealth/ptsd.html
https://kidshealth.org/en/parents/ptsd.html
https://childmind.org/guide/post-traumatic-stress-disorder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1414752
https://adaa.org/living-with-anxiety/children/posttraumatic-stress-disorder-ptsd/symptoms
https://www.e-counseling.com/ptsd/things-not-to-say-to-someone-with-ptsd
Book Recommendations:
Children and Trauma: A Guide for Parents and Professionals by Cynthia Monahon
Trauma Through a Child's Eyes: Awakening the Ordinary Miracle of Healing by Maggie Kline and Peter A. Levine
Integrative Parenting: Strategies for Raising Children Affected by Attachment Trauma by Cathy Schweitzer, Debra Wesselmann, and Stefanie Armstrong
Creating Loving Attachments by Daniel A. Hughes and Kim Golding
It Didn't Start With You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle by Mark Wolynn
Professionals diagnose Acute Stress Disorder when an individual exhibits a particularly strong and long-lasting response to a distressing event, such as a death, injury, or natural disaster. This reaction can last up to a month following the distressing event and may result in an inability to function at home, at school, and with peers. If the response lasts longer than one month, the diagnosis of Post-Traumatic Stress Disorder should then be considered.
Internet Resources:
Resources vary based on the distressing event. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the distressing event. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Adjustment Disorder is diagnosed when an individual exhibits a particularly strong and longstanding emotional or behavioral responses to non-life threatening stress or change. Examples include:
-
-
-
- Moving
- Death of a loved one or beloved pet
- Parental divorce or separation
- A new sibling
- A sudden or chronic illness in the individual or loved one
-
-
Please visit the following sites for more information regarding:
https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P01573
https://childmind.org/guide/guide-adjustment-disorder
https://www.chop.edu/conditions-diseases/adjustment-disorders
https://www.hopkinsmedicine.org/health/conditions-and-diseases/adjustment-disorders
https://www.mayoclinic.org/diseases-conditions/adjustment-disorders/diagnosis-treatment/drc-20355230
Internet Resources:
Resources vary based on the stressor. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the stressor. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Somatic Symptom and Related Disorders
Somatic Symptom and Related Disorders are a set of diagnoses characterized by physical pain and symptoms that a person feels, which are caused (or mostly caused) by psychological factors. Medical results and tests cannot explain the symptoms or the symptom severity.
Professionals diagnose Somatic Symptom Disorder when a person is preoccupied with illness and ruminates about the potential for getting sick for a significant period of time each week. In turn, high levels of anxiety result in physical symptoms like lethargy, stomach pain, nausea, and headaches, which may serve as further confirmation that there is something wrong.
Please visit the following sites for more information regarding Somatic Symptom Disorder:
https://childmind.org/guide/somatic-symptom-disorder
https://www.aboutkidshealth.ca/article?contentid=3668&language=english
Book Recommendations:
When Your Child Hurts: Effective Strategies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain 1st Edition by Rachael Coakley
Illness Anxiety Disorder is diagnosed when a person exhibits a preoccupation with severe medical issues, although there are mild or no symptoms. Moreover, these individuals are not reassured by medical professionals or test results indicating that they are healthy.
Please visit the following sites for more information regarding Illness Anxiety Disorder:
https://childmind.org/article/quick-facts-illness-anxiety-disorder
https://www.health.harvard.edu/a_to_z/illness-anxiety-disorder-a-to-z
https://my.clevelandclinic.org/health/diseases/9886-illness-anxiety-disorder-beyond-hypochondriasis
Book Recommendations:
When Your Child Hurts: Effective Strategies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain 1st Edition by Rachael Coakley
A Kids Book About Anxiety by Ross Szabo
Freeing Your Child from Negative Thinking: Powerful, Practical Strategies to Build a Lifetime of Resilience, Flexibility, and Happiness by Tamar Chansky
Freeing Your Child from Anxiety by Tamar Chansky
Parenting the New Teen in the Age of Anxiety by John Duffy
Helping Your Anxious Child by Ronald Rapee, Ann Wignall, Susan Spencer, et al.
Professionals diagnose Conversion Disorder (Functional Neurological Symptom Disorder) when individuals exhibit difficulties with their sensory or preceptory systems like numbness, paralysis, seizures, blindness, or deafness that cannot be attributed to a medical cause or injury. These symptoms are not artificial or imagined. Moreover, they directly impact the body’s ability to function.
Please visit the following sites for more information regarding Conversion Disorder (Functional Neurological Symptom Disorder):
https://www.chop.edu/conditions-diseases/conversion-disorder
https://my.clevelandclinic.org/health/diseases/17787-conversion-disorder-in-children--adolescents
https://www.mayoclinic.org/diseases-conditions/conversion-disorder/symptoms-causes/syc-20355197
https://www.health.harvard.edu/newsletter_article/Conversion_disorder
https://www.psychologytoday.com/us/blog/the-author-speaks/201811/conversion-disorder
Book Recommendations:
Conversion Disorder by Jesse Russell and Ronald Cohn
When Your Child Hurts: Effective Strategies to Increase Comfort, Reduce Stress, and Break the Cycle of Chronic Pain 1st Edition by Rachael Coakley
A Kids Book About Anxiety by Ross Szabo
Freeing Your Child from Negative Thinking: Powerful, Practical Strategies to Build a Lifetime of Resilience, Flexibility, and Happiness by Tamar Chansky
Freeing Your Child from Anxiety by Tamar Chansky
Parenting the New Teen in the Age of Anxiety by John Duffy
Helping Your Anxious Child by Ronald Rapee, Ann Wignall, Susan Spencer, et al.
Feeding and Eating Disorders
Feeding and Eating Disorders are a group of diagnoses characterized by maladaptive eating behaviors that result in health and psychosocial problems.
Professionals diagnose Pica Disorder when an individual routinely eats non-nutritive food items (e.g., rocks, dirt, crayons, paper clips, human waste). Sometimes Pica occurs due to identifiable stressors, cultural factors, nutritional deficiencies, or pregnancy.
Please visit the following sites for more information regarding Pica Disorder:
https://kidshealth.org/en/parents/pica.html
https://www.hopkinsallchildrens.org/Patients-Families/Health-Library/HealthDocNew/Pica
https://www.nationaleatingdisorders.org/learn/by-eating-disorder/other/pica
https://www.healthline.com/health/pica
https://www.superkidsnutrition.com/pica-in-toddlers-and-preschoolers
Book Recommendations:
Craving Earth: Understanding Pica--The Urge to Eat Clay, Starch, Ice, and Chalk by Sera L. Young
Professionals diagnose Rumination Disorder when a person, usually an infant or young child, vomits and re-chews food that was already swallowed. For this diagnosis to be made, symptoms must be present for at least one month and cannot be attributed to another medical condition (e.g., acid reflux).
Please visit the following sites for more information regarding Rumination Disorder:
https://www.chop.edu/conditions-diseases/rumination-syndrome
https://www.aboutkidsgi.org/rumination-syndrome.html
https://www.stlouischildrens.org/conditions-treatments/rumination-syndrome
https://www.nationwidechildrens.org/conditions/rumination-syndrome
https://www.mayoclinic.org/diseases-conditions/rumination-syndrome/symptoms-causes/syc-20377330
Book Recommendations:
How to Nourish Your Child Through an Eating Disorder: A Simple, Plate-by-Plate Approach to Rebuilding a Healthy Relationship with Food by Casey Crosbie Wendy Sterling
Rumination Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related Conditions by Kenneth Kee
Ovis Has Trouble with Eating by Kelly Beins
Avoidant/Restrictive Food Intake Disorder is diagnosed when individuals exhibit resistance to, or fear of, eating that cannot be attributed to another medical condition. Examples include, but are not limited to, a fear of eating in front of others or of eating alone, an irrational fear of choking, and refusal to eat most or all foods. These maladaptive behaviors can result in delayed growth, and can lead to severe health complications.
Please visit the following sites for more information regarding Avoidant/Restrictive Food Intake Disorder:
https://www.aboutkidshealth.ca/article?contentid=275&language=english
https://www.nationaleatingdisorders.org/blog/more-picky-eating%E2%80%947-things-know-about-arfid
https://www.eatingdisorderhope.com/blog/parenting-arfid-warning-signs-treatment-options
Book Recommendations:
Helping Your Child with Extreme Picky Eating: A Step-by-Step Guide for Overcoming Selective Eating, Food Aversion, and Feeding Disorders by Jenny McGlothlin and Katja Rowell
Food Refusal and Avoidant Eating in Children, Including Those with Autism Spectrum Conditions: A Practical Guide for Parents and Professionals by Elizabeth Shea and Gillian Harris
Food Chaining: The Proven 6-Step Plan to Stop Picky Eating, Solve Feeding Problems, and Expand Your Child's Diet by Cheryl Fraker, Mark Fishbein, Sibyl Cox, and Laura Walbert
Try New Food: How to Help Picky Eaters Taste, Eat & Like New Foods by Jill Castle
Anorexia Nervosa is an eating disorder characterized by intense fear of gaining weight and persistent behaviors that interfere with weight gain, even though the individual is underweight. Those with this diagnosis experience a disturbance in the way in which they perceive their weight and body image. There are two types of Anorexia Nervosa:
Restrictor Type: This is defined by severe restrictions in food an individual eats, especially those high in carbohydrates and fats.
Bulimic (binging and purging) Type: Individuals with this type will often overeat and then force themselves to throw up. They may also take heavy doses of laxatives or other medications that clear out their digestive system. Unlike individuals with Bulimia Nervosa who are of normal weight or who are overweight, those with Anorexia Nervosa binge-eating/purging type are underweight.
Please visit the following sites for more information regarding Anorexia Nervosa:
https://www.stanfordchildrens.org/en/topic/default?id=anorexia-nervosa-in-children-90-P02554
https://www.nationaleatingdisorders.org/help-support/contact-helpline
https://childmind.org/guide/guide-to-anorexia-nervosa
https://kidshealth.org/ChildrensHealthNetwork/en/parents/az-anorexia.html
Book Recommendations:
The Upside of Being Down : The Life of a Teen with Anorexia by Caroline Rodriguez
Eating Disorders: A Question and Answer Book about Anorexia Nervosa and Bulimia Nervosa by Ellen Erlanger
Reversing Your Child's Eating Disorder: Healing a Hijacked Mind to Overcome Anorexiaby Jessica Goering
Unpack Your Eating Disorder: The Journey to Recovery for Adolescents in Treatment for Anorexia Nervosa and Atypical Anorexia Nervosa by Maria Ganci and Lindsey Atkins
The Disappearing Sister: The Story of a Child's View on Dealing with Anorexia Nervosa by Elizabeth Cummings
Hunger for Understanding: A Workbook for Helping Young People to Understand and Overcome Anorexia Nervosa by Alison Eivors and Sophie Nesbitt
My Kid is Back: Empowering Parents to Beat Anorexia Nervosa by June Alexander
Bulimia Nervosa is an eating disorder characterized by high levels of overeating offset by fasting, extreme exercise, or purging. Individuals with Bulimia Nervosa generally maintain an average or above weight, unlike those with Anorexia Nervosa who typically experience below average weight. This diagnosis generally expresses itself in late adolescence or early adulthood, and is commonly connected with societal goals of beauty and attractiveness.
Please visit the following sites for more information regarding Bulimia Nervosa:
https://childmind.org/guide/bulimia-nervosa-guide/
https://www.nationaleatingdisorders.org/help-support/contact-helpline
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P01592
http://www.childrenshospital.org/conditions-and-treatments/conditions/b/bulimia-nervosa
https://www.eatingdisorderhope.com/information/bulimia/caring-for-a-child-with-bulimia-nervosa
https://www.nationwidechildrens.org/conditions/bulimia-nervosa
https://www.childrens.com/specialties-services/conditions/bulimia
Book Recommendations:
Why Are They Starving Themselves?: Understanding Anorexia Nervosa and Bulimia by Elaine Landau
Anorexia and Bulimia: Control That Is Out of Control by June Hunt
Healthy Body Image: Teaching Kids to Eat and Love Their Bodies Too! by Kathy Kater
When Your Teen Has an Eating Disorder: Practical Strategies to Help Your Teen Recover from Anorexia, Bulimia, and Binge Eating by Lauren Muhlheim
Why Can't I Look The Way I Want? Overcoming Eating Issues by Melinda Hutchings
Bulimic To Believer: Using Biblical Principals to Understand Why Bulimia is More than Eating Disorder by Jamella Stroud
Binge-Eating Disorder is diagnosed when an individual repeatedly consumes very large amounts of food in a short period. Typically, the behavior is impulsive and followed by feelings of shame, regret, and guilt. People who suffer from Binge-Eating Disorder typically are of average or above weight. For this diagnosis to be made, purging behaviors do not occur.
Please visit the following sites for more information regarding Binge-Eating Disorder:
https://childmind.org/guide/guide-to-binge-eating-disorder
https://www.nationaleatingdisorders.org/help-support/contact-helpline
https://kidshealth.org/en/parents/binge-eating.html
https://www.eatingdisorderhope.com/information/binge-eating-disorder/children-adolescents
Book Recommendations:
When Your Teen Has an Eating Disorder: Practical Strategies to Help Your Teen Recover from Anorexia, Bulimia, and Binge Eating by Lauren Muhlheim
Overeating : Understanding, Overcoming and Preventing Overeating, Binge Eating, Body Image Problems, Emotional Eating and Diet Troubles by Robert Lee
Emotional Overeating: No Binge Again! A Journey Through Your Emotions to Master and Stop Emotional Eating and Compulsive Overeating by Emily Collins
Why Can't You Just Eat? : A Look Inside the Mind of Anorexia, Bulimia, and Binge Eating Disorder by Shannon Lagasse
Elimination Disorders
Elimination Disorders are a set of diagnoses characterized by inappropriate elimination of urine or feces, typically beginning in childhood or adolescence. These behaviors may be voluntary or involuntary.
Enuresis is diagnosed when an individual (age 5 and older) repeatedly urinates in a place other than the toilet (e.g., bed, clothing, floor), whether intentionally or unintentionally. Some may be entirely unaware of their need to go to the bathroom or become distracted until it is too late. For others, they may hold their urine for varying reasons (e.g., feeling of control, not wanting to use a public restroom) and have an accident. At times, voiding of urine in inappropriate places may be a sign of a behavioral problem.
Please visit the following sites for more information regarding Enuresis:
https://childmind.org/guide/guide-to-enuresis
https://www.mayoclinic.org/diseases-conditions/bed-wetting/symptoms-causes/syc-20366685
https://www.mottchildren.org/health-library/ta2112
Book Recommendations:
Waking Up Dry: A Guide to Help Children Overcome Bedwetting by Howard J. Bennett
Seven Steps to Nighttime Dryness: A Practical Guide for Parents of Children with Bedwetting by Renee Mercer
Getting To Dry: How to Help Your Child Overcome Bedwetting by Barbara Keating, Diane Rosenbaum, and Max Maizels
Sammy the Elephant & Mr. Camel: A Story to Help Children Overcome Enuresis While Discovering Self-Appreciation by Joyce Mills and Richard Crowley
The Complete Bedwetting Book: Including a Daytime Program for Nighttime Dryness by Preston Smith and Michelle Passamaneck
Encopresis is diagnosed when an individual (age 5 and older) repeatedly defecates in a place other than the toilet (e.g., bed, clothing, floor), whether intentionally or unintentionally. Some may be entirely unaware of their need to go to the bathroom or become distracted until it is too late. For others, they may hold their bowels for varying reasons (e.g., feeling of control, not wanting to use a public restroom) and have an accident. At times, voiding of bowels in inappropriate places may be a sign of a behavioral problem.
Please visit the following sites for more information regarding Encopresis:
https://childmind.org/guide/guide-to-encopresis
https://kidshealth.org/en/parents/encopresis.html
https://www.mayoclinic.org/diseases-conditions/encopresis/symptoms-causes/syc-20354494
https://www.chop.edu/conditions-diseases/encopresis
https://www.cincinnatichildrens.org/health/e/encopresis
https://www.stanfordchildrens.org/en/topic/default?id=encopresis-90-P01992
http://www.childrenshospital.org/conditions-and-treatments/conditions/e/encopresis
Book Recommendations:
I Can't, I Won't, No Way! A Book for Children Who Refuse to Poop by Tracey J. Vessillo
Constipation, Withholding and Your Child: A Family Guide to Soiling and Wetting by Anthony Cohn
Encopresis‑‑ You Can Beat It! Game‑Changing Solutions for Toilet Anxiety, Soiling, and Constipation by Baruch Kushnir
It Hurts when I Poop! A Story for Children who are Scared to Use the Potty The Potty Wars: Understanding and Helping Your Encopretic Child by Libby Robbins by Howard J. Bennett
Sleep-Wake Disorders
Sleep-Wake Disorders are a set of diagnoses characterized by impairment in the quality or quantity of sleep an individual receives. Difficulty falling or staying asleep, waking up in the morning, daytime fatigue, teeth-grinding during sleep, bedwetting, recurrent nightmares, and difficulty breathing while asleep can all be signs of Sleep-Wake Disorders. When one or more of these symptoms occur regularly, it can have detrimental effects on a person’s mood and ability to function throughout the day.
Individuals are diagnosed with Insomnia Disorder when they persistently experience difficulty falling or staying asleep at nighttime, or awakening too early in the morning. While everyone experiences disruptions in sleep from time to time due to stressor, sickness, changes in medication, etc., Insomnia Disorder is diagnosed when an individual persistently exhibits these difficulties three or more times per week for at least one month.
Please visit the following sites for more information regarding Insomnia Disorder:
https://childmind.org/article/quick-facts-on-insomnia
https://my.clevelandclinic.org/health/diseases/14301-insomnia-in-children
http://sleepeducation.org/sleep-disorders-by-category/insomnias/child-insomnia
http://www.childrenshospital.org/conditions-and-treatments/conditions/i/insomnia/symptoms-and-causes
https://www.behavioralsleep.org/index.php/sbsm/about-childhood-sleep-disorders/childhood-insomnia
https://www.helpguide.org/articles/sleep/childhood-insomnia-and-sleep-problems.htm
https://healthmatch.io/insomnia
Book Recommendations:
Sleep in Children and Adolescents by Mary Carskadon and Oskar G. Jenni
Solve Your Child's Sleep Problems: New, Revised, and Expanded Edition by Richard Ferber
The Sleep Book for Tired Parents : Help for Solving Children's Sleep Problems by Rebecca Huntley
Healthy Sleep Habits, Happy Child by Marc Weissbluth
The Baby Sleep Solution: A Proven Program to Teach Your Baby to Sleep Twelve Hours a Night by Lisa Abidin and Suzy Giordano
Professionals diagnose Hypersomnolence Disorder when an individual persistently sleeps for a significant number of hours per night and/or experience frequent sleepiness throughout the day despite achieving adequate sleep. Moreover, napping does not relieve the symptoms of daytime fatigue. Individuals with Hypersomnolence Disorder frequently feel disoriented upon awakening. There are various causes, such as substance abuse, other sleep disorders, and medical conditions. Effects of Hypersomnolence Disorder are wide ranging and can include, but are not limited to:
-
-
-
- Appetite and weight disturbances
- Difficulties with focus and attention
- Low energy
- Heightened stress response and emotion regulation difficulties
- Hallucinations
-
-
Please visit the following sites for more information regarding Hypersomnolence Disorder:
https://www.childneurologyfoundation.org/disorder/hypersomnia
https://www.childrens.com/specialties-services/conditions/excessive-daytime-sleepiness
https://www.childrensmn.org/educationmaterials/childrensmn/article/18037/hypersomnia
https://www.psychologytoday.com/us/conditions/hypersomnolence
Internet Resources:
Resources vary based on the reason for hypersomnolence. As such, please ask your neuropsychologist directly for internet resources appropriate for your child’s needs. Contact Us
Book Recommendations:
Book recommendations vary based on the reason for hypersomnolence. As such, please ask your neuropsychologist directly for book recommendations appropriate for your child’s needs. Contact Us
Narcolepsy is a neurological disorder that affects the brain’s ability to control sleep and wakefulness, resulting in overwhelming daytime fatigue that severely impacts a person’s functioning. There are two types of narcolepsy:
Narcolepsy Type 1: Individuals with Narcolepsy Type 1 experience extreme sleepiness during the day because of low levels of orexin (also known as hypocretin), which is a neuropeptide that regulates arousal, wakefulness, and appetite. Cataplexy (i.e., a sudden and uncontrollable muscle weakness or paralysis that comes on during the day and is often triggered by a strong emotion, such as excitement or laughter) can also occur.
Narcolepsy Type 2: Individuals with Narcolepsy Type 2 also have extreme sleepiness during the day but do not express cataplexy or high levels of orexin.
Please visit the following sites for more information regarding Narcolepsy:
https://my.clevelandclinic.org/health/diseases/14307-narcolepsy-in-children
https://www.chop.edu/conditions-diseases/narcolepsy
https://www.ajmc.com/newsroom/pediatric-narcolepsy-symptoms-differ-from-those-of-adults-review-finds
Book Recommendations:
Narcolepsy: A Funny Disorder That's No Laughing Matter by Marguerite J. Utley
Sometimes My Socks Are in the Freezer by Amanda Stock
Solve Your Child's Sleep Problems: New, Revised, and Expanded Edition by Richard Ferber
Obstructive Sleep Apnea is diagnosed when an individual exhibits recurrent interruptions in breathing while asleep. In most cases, the interruption is due to a blockage (e.g., enlarged tonsils or adenoids) or decreased muscle tone resulting in the breathing passageways becoming narrower. Obstructive Sleep Apnea in the pediatric population is most common in children between ages two and six years, but can occur at any age.
Please visit the following sites for more information regarding Obstructive Sleep Apnea:
https://www.chop.edu/conditions-diseases/obstructive-sleep-apnea
https://www.mayoclinic.org/diseases-conditions/pediatric-sleep-apnea/symptoms-causes/syc-20376196
https://kidshealth.org/en/parents/apnea.html
https://www.sleepapnea.org/treat/childrens-sleep-apnea
https://my.clevelandclinic.org/health/diseases/14312-obstructive-sleep-apnea-in-children
Book Recommendations:
Sleep Apnea in Children: A Handbook for Families by David Ingram
My Tired Brain: A Child's Journey to Understanding Sleep Apnea by Angela Deal
Sleep with Buteyko: Stop Snoring, Sleep Apnoea and Insomnia. Suitable for Children and Adults by Patrick McKeown
Professionals diagnose Central Sleep Apnea when they observe an interruption in breathing while an individual is asleep that typically is not accompanied by gasping or snoring. This diagnosis is caused by a malfunction in the medulla oblongata (i.e., region of the brain responsible for inhalation and exhalation). Over time, this problem can lead to significant sleep disruptions and a lack of oxygen to the brain. Central Sleep Apnea is more commonly observed in high altitudes.
Please visit the following sites for more information regarding Central Sleep Apnea:
https://www.healthline.com/health/sleep-apnea-in-children
https://kidshealth.org/Nemours/en/parents/101554.html?WT.ac=ctg
https://www.childrensmn.org/educationmaterials/childrensmn/article/18039/central-sleep-apnea-
Book Recommendations:
Sleep Apnea in Children: A Handbook for Families by David Ingram
My Tired Brain: A Child's Journey to Understanding Sleep Apnea by Angela Deal
Sleep with Buteyko: Stop Snoring, Sleep Apnea and Insomnia. Suitable for Children and Adults by Patrick McKeown
A Circadian Rhythm Sleep-Wake Disorder is diagnosed when there is a persistent disruption in the timing of a person’s internal sleep-wake rhythm (i.e., circadian rhythm) that interferes with their restorative sleep and, subsequently, their functioning throughout the day. Research has shown that the human body has an internal clock (i.e., suprachiasmatic nucleus) that regulates the 24-hour circadian rhythm and is “set” by light and darkness. Circadian rhythms and their sensitivity to time cues may change as a person ages.
There are various types of Circadian Rhythm Sleep-Wake Disorders:
Delayed Sleep-Wake Phase: Occurs when the sleep cycle is delayed by two or more hours, resulting in a person going to sleep later at night and sleeps later in the morning.
Advanced Sleep-Wake Phase: Occurs when the initiation of the sleep cycle is expedited, resulting in a person falling asleep several hours before a normal bedtime and waking up hours earlier.
Irregular Sleep-Wake Rhythm: Occurs when a person's circadian rhythm is so disorganized that there is no clear indication of a sleep or wake pattern.
Non-24-Hour Sleep-Wake Rhythm: Occurs when a person's sleep cycle is shifted a little later every day.
Shift Work: Occurs when a non-traditional work schedule interferes with an individual’s circadian rhythm.
Jet lag: Occurs when an individual travels across multiple time zones and has difficulty adjusting to the new schedule.
Please visit the following sites for more information regarding Circadian Rhythm Sleep-Wake Disorder:
http://sleepeducation.org/sleep-disorders-by-category/circadian-rhythm-disorders
https://my.clevelandclinic.org/health/diseases/12115-circadian-rhythm-disorders
https://www.childrens.com/specialties-services/conditions/circadian-rhythm-disorder
https://www.mdedge.com/psychiatry/article/62088/when-child-cant-sleep-start-treating-parents
https://www.circadiansleepdisorders.org/defs.php
Book Recommendations:
Sleep in Children and Adolescents by Mary Carskadon and Oskar G. Jenni
Solve Your Child's Sleep Problems: New, Revised, and Expanded Edition by Richard Ferber
The Sleep Book for Tired Parents : Help for Solving Children's Sleep Problems by Rebecca Huntley
Healthy Sleep Habits, Happy Child by Marc Weissbluth
The Baby Sleep Solution: A Proven Program to Teach Your Baby to Sleep Twelve Hours a Night by Lisa Abidin and Suzy Giordano
To better understand this diagnosis, you should first have a foundational understanding of sleep cycles in general. Read More
When asleep, a person cycles between REM (rapid eye movement) and various stages of NREM (non-rapid eye movement) sleep, with each complete cycle lasting for approximately 90-120 minutes. NREM Sleep: There are three phases of non-REM sleep, each of which ranges from five to fifteen minutes. A person goes through all three stages of NREM sleep before entering into REM sleep. Stage 1: A person’s eyes are closed, but it is easy for them to wake up. Stage 2: A person is in a “light sleep,” where their heart rate slows and their body temperature drops. Stages 3: This is the “deep sleep” stage. The body repairs and regrows tissues, builds bone and muscle, and strengthens the immune system. It is difficult to rouse a person during this stage. REM Sleep: During REM sleep, the brain is more active. A person’s heart rate and breathing increase, and more intense dreams occur. REM sleep occurs approximately 90 minutes after a person falls asleep. The first period of REM sleep typically lasts 10 minutes. Each subsequent REM stages gets longer. Now that you have a better understanding of sleep cycles, let’s talk about Non-Rapid Eye Movement (NREM) Sleep Arousal Disorders. This set of diagnoses refer to repeated episodes of incomplete awakening and usually happen during the first third of the night. People with this condition have no memory of their dreams or sleep behavior in the morning. NREM sleep arousal disorders occur most commonly in childhood and happen less frequently as a person matures age; however, this is not always the case. There are three types of NREM Sleep Arousal Disorders: Confusional Arousals: Occurs when the person wakes up in a confused state. Sleep-Walking: Occurs when the person sits up or gets out of bed and walks around when asleep. Sleep Terrors: Occurs when a person appears to be awake but is actually asleep and experiences a severe sense of panic, which cannot be consoled. Please visit the following sites to learn for more information regarding Non-Rapid Eye Movement (NREM) Sleep Arousal Disorders: https://www.mindyra.com/solutions/child/non-rapideyemovementsleeparousal https://kidshealth.org/en/parents/terrors.html https://www.sleepfoundation.org/articles/night-terrors-when-talk-doctor https://www.sleepfoundation.org/articles/sleepwalking https://www.mayoclinic.org/diseases-conditions/sleepwalking/symptoms-causes/syc-20353506 https://www.nationwidechildrens.org/conditions/sleep-terrors-and-sleepwalking Book Recommendations: The Nocturnal Brain: Nightmares, Neuroscience, and the Secret World of Sleep by Guy Leschziner Mommy, Daddy, I Had a Bad Dream! by Martha Heineman Solve Your Child's Sleep Problems: New, Revised, and Expanded Edition by Richard Ferber Helping Your Child with Sleep Problems: A Self-Help Guide for Parents by Rachel Miller and Michael Gradisar Take Charge of Your Child's Sleep: The All-in-One Resource for Solving Sleep Problems in Kids and Teens by Judy Owens and Jodi Mindell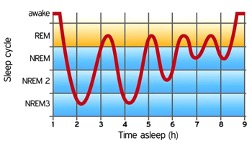
https://www.scienceabc.com/eyeopeners/why-is-sleep-important.html
Occasional nightmares are normal and tend to decrease with age. However, professionals diagnose Nightmare Disorder when an individual exhibits consistent and persistent nightmares that result in sleep disruption, extreme distress, and/or a fear of sleeping.
Please visit the following sites for more information regarding Nightmare Disorder:
https://www.mayoclinic.org/diseases-conditions/nightmare-disorder/symptoms-causes/syc-20353515
https://www.sleepfoundation.org/articles/children-and-bedtime-fears-and-nightmares
https://www.sleepfoundation.org/articles/nightmares-and-sleep
http://sleepeducation.org/sleep-disorders-by-category/parasomnias/nightmares/risk-factors
Book Recommendations:
How to Knock Out Nightmares by Catherine Leblanc and Roland Garrigue
Mommy, Daddy, I Had a Bad Dream! by Martha Heineman Pieper
A Terrible Thing Happened by Margaret Holmes
Everything You Need to Know About NIGHTMARES! and How to Defeat Them: The Nightmares! Handbook by Jason Segel and Kirsten Miller
Tiger vs. Nightmare by Emily Tetri
Neon the Ninja Activity Book for Children Who Struggle with Sleep and Nightmares: A Therapeutic Story with Creative Activities for Children Aged 5-10 by Karen Treisman
Gender Dysphoria
Gender Dysphoria refers to extreme discomfort caused by a discrepancy between a person’s gender at birth (called assigned gender) and the gender they feel themselves to be (affirmed gender). Extreme distress is experienced when gender dysphoria occurs, as the individual often feels as though they are “trapped” in the wrong body. Severe instances can lead to suicidal ideation, self-harm, depression, and anxiety when left unresolved. Of note, the individual’s affirmed gender is NOT what is being diagnosed – rather their discontent with their assigned gender is classified as problematic.
Please visit the following sites for more information about Gender Dysphoria:
https://childmind.org/guide/guide-to-gender-dysphoria
https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria
Book Recommendations:
The Gender Creative Child: Pathways for Nurturing and Supporting Children Who Live Outside Gender Boxes by Diane Ehrensaft
The Transgender Child: A Handbook for Families and Professionals by Stephanie Brill Gender Born, Gender Made: Raising Healthy Gender-Nonconforming Children by Diane Ehrensaft
Raising My Rainbow: Adventures in Raising a Fabulous, Gender Creative Son by Lori Duron
The Conscious Parent's Guide to Gender Identity: A Mindful Approach to Embracing Your Child's Authentic Self by Darlene Tando
I Am Jazz by Jessica Herthel
Jacob's New Dress by Ian Hoffman and Sarah Hoffman
Transgender Teen by Stephanie Brill
Who Are You? The Kid's Guide to Gender Identity by Brook Pessin-Whedbee
Substance-Related Disorders
Substance-Related Disorders are a set of diagnoses characterized by an overuse of drugs or alcohol, which negatively impacts a person’s functioning across settings (e.g., school, home, extra-curricular activities, time with friends/family). Research shows that substances directly activate the brain’s reward system, which can result in feelings of pleasure. Of note, the specific pleasurable feelings evoked can vary widely depending on the drug and the individual.
Alcohol-Related Disorder is diagnosed when there is a pattern of alcohol use that includes a preoccupation with alcohol, unhealthy consumption of alcohol, drinking more heavily and more often without feeling as inebriated, and experiencing withdrawal symptoms when drinking is stopped. Binge drinking may also be experienced.
Please visit the following sites for more information regarding Alcohol-Related Disorder:
https://www.addictionguide.com/alcohol
https://www.mcleanhospital.org/news/what-you-need-know-about-alcohol-and-developing-teenage-brain
https://www.mayoclinic.org/diseases-conditions/alcohol-use-disorder/symptoms-causes/syc-20369243
https://www.alcohol.org/comorbid/neurologic-desease
https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm
Book Recommendations:
Teens Talk about Alcohol and Alcoholism by Paul Dolmetsch and Gain Mauricette
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth About Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor
Professionals diagnose Cannabis-Related Disorder when they observe abusive use of cannabis in an individual. Tetrahydrocannabinol (THC) in cannabis causes it to be addictive to the user and, once it hits the bloodstream, the individual feels "high." In the United States, around 5 percent of people over the age of twelve have a Cannabis-Related Disorder. It interferes with functionality and quality of life, as well as one’s drive and determination.
Please visit the following sites for more information regarding Cannabis-Related Disorder:
https://www.addictionguide.com/addiction
https://americanaddictioncenters.org/marijuana-rehab/effects-of-marijuana-on-teenage-brain
https://www.pnas.org/content/117/1/7
https://www.apa.org/monitor/2015/11/marijuana-brain
https://www.gulfbend.org/poc/view_doc.php?type=doc&id=48505&cn=1408
Book Recommendations:
The Teenage Brain: A Neuroscientist's Survival Guide to Raising Adolescents and Young Adults by Frances Jensen and Amy Ellis Nutt
The Cannabis Craze: A Practical Guide for Parents and Teens by Marc Aronoff
Tell Your Children: The Truth About Marijuana, Mental Illness, and Violence by Alex Berenson
Marijuana's Harmful Effects on Youth by Julie Nelson
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth About Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor
Professionals diagnose Tobacco-Related Disorder when they observe an addiction to tobacco and/or tobacco-related products in an individual. Nicotine, a highly addictive chemical, leads to substance dependence and a desire to ingest more despite knowing the harm it causes. Tobacco-Related Disorder occurs more often than any other substance abuse diagnosis in the United States, and it can cause disability and early death. Second-hand smoke can impact others in the area who are not smoking.
Please visit the following sites for more information regarding Tobacco-Related Disorder:
https://www.psychologytoday.com/us/conditions/tobacco-related-disorders
https://teen.smokefree.gov/the-risks-of-tobacco/nicotine-addiction
https://tobaccofreeca.com/e-cigarettes/the-effects-of-nicotine-on-the-adolescent-brain
https://e-cigarettes.surgeongeneral.gov/knowtherisks.html
https://www.sciencenewsforstudents.org/article/explainer-nico-teen-brain
Book Recommendations:
Facts for Teenagers; Smoking, Health, and You by The United States Children’s Bureau
How to Stop Your Child Smoking by Allen Carr
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth about Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor
Professionals diagnose Stimulant-Related Disorder when they observe dependency on stimulants or withdrawal from stimulants. These drugs heighten attention, focus, alertness, and energy. They can be appropriately prescribed for medical conditions (e.g., to treat obesity, ADHD, narcolepsy, and depression), but they are dangerous when used recreationally. Examples include methamphetamine, cocaine, and amphetamines.
Please visit the following sites for more information regarding Stimulant-Related Disorder:
https://www.addictionguide.com/addiction
https://www.psychologytoday.com/us/conditions/stimulant-related-disorders
https://www.addictioncenter.com/stimulants
https://www.drugabuse.gov/publications/drugfacts/prescription-stimulants
https://www.drugabuse.gov/publications/drugfacts/cocaine
Book Recommendations:
Addicted to Perfect: A Journey Out of the Grips of Adderall by Vitale Buford
Methamphetamine And Stimulant Abuse by Bethany Bryan
A Parent's Guide to Teen Addiction: Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth About Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor
Professionals diagnose Hallucinogen-Related Disorder when an individual exhibits dependency on hallucinogens or withdrawal when attempting to stop. Hallucinogens change sensory perception, cognition, and the affective state of the individual. Individuals may experience a feeling of divinity or transcendence. Withdrawal may lead to a state of delirium. Temporary or permanent disruptions can be observed in body orientation, intelligence, judgment, memory retrieval, and/or emotions.
Please visit the following sites for more information regarding Hallucinogen-Related Disorder:
https://www.healthychildren.org/English/ages-stages/teen/substance-abuse/Pages/Hallucinogens.aspx
https://www.drugabuse.gov/drug-topics/hallucinogens
https://store.samhsa.gov/product/Tips-for-Teens-The-Truth-About-Hallucinogens/PEP20-03-03-001
https://www.drugabuse.gov/publications/drugfacts/hallucinogens
Book Recommendations:
Hallucinogens: The Effects of Drug Abuse on Children & Teens by Dr. J. Frederick Garman and Waln Brown
LSD, PCP, and Hallucinogen Drug Dangers by Judy Monroe
A Parent's Guide to Teen Addiction: Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth About Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor
Professionals diagnose Opioid-Related Disorder when they observe a dependence on drugs meant to treat pain caused by an acute injury, illness, or surgery. These may be natural or manufactured substances. Examples include, but are not limited to, Cargentanil, Pethidine, Methadone, Tramadol, and Fentanyl. At high doses, opioids can result in euphoria. Side effects of generally include digestive issues, and disorientation, as well as death in severe cases.
Please visit the following sites for more information regarding Opioid-Related Disorder:
https://www.addictionguide.com/addiction
https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder/opioid-use-disorder
https://www.drugabuse.gov/drug-topics/opioids
https://www.drugabuse.gov/publications/opioid-facts-teens/letter-to-teens
https://www.campusdrugprevention.gov/sites/default/files/WH-Youth-Opioid-Prevention-Brocure.pdf
Book Recommendations:
Thinking Critically: Opioid Abuse by Christine Wilcox
Let's Make A Contract: Getting Your Teen Past Opioid by Ann Schiebert
A Parent's Guide to Teen Addiction: Professional Advice on Signs, Symptoms, What to Say, and How to Help by Laurence M. Westreich
Choices and Consequences: What to Do When a Teenager Uses Alcohol/Drugs by Dick Schaefer
Teens Under the Influence: The Truth About Kids, Alcohol, and Other Drugs-- how to Recognize the Problem and What to Do About It by Katherine Ketcham and Nicholas Pace
Substance Abuse: The Ultimate Teen Guide by Sheri Mabry Bestor